Disease Information
Type 1 Diabetes
Type 1 diabetes is also known as juvenile diabetes or insulin-dependent diabetes. It is a chronic condition where pancreas secretes little or no insulin, a hormone required to allow sugar (glucose) to enter cells to produce energy. On the other hand type 2 diabetes results when the body becomes resistant to the effects of insulin or it secretes less of insulin.
Type 1 diabetes may occur due to various factors, which may include genetics and contact to certain viruses. Generally type 1 diabetes typically appears during childhood or adolescence, but it can also develop in adults. There is no cure for type 1 diabetes but still it can be managed. People who have type 1 diabetes can expect to live longer and healthier lives with proper treatment

The exact cause for type 1 diabetes is still not known. Type 1 diabetes may occur due to dysfunctioning of the body's own immune system which mistakenly destroys the insulin-producing (islet) cells in the pancreas. This process may be because of genetics or exposure to certain viruses
The role of insulin
Insulin is one of the hormones that is secreted from the islets cells of pancreas, a gland to be found behind and below the stomach. When the islet cells are destroyed, there will be little or no insulin.
- Insulin is secreted from pancreas into the bloodstream.
- The circulating insulin helps sugar enter into cells
- Amount of sugar in ones bloodstream is lowered by insulin.
- Whenever blood sugar level drops, the secretion of insulin from pancreas also reduces.
The role of glucose
Glucose is a sugar which is one of the main sources of energy for the body cells that build up muscles and other tissues.
- Food and our liver are two main sources of glucose.
- Sugar from bloodstream enters inside the cells with the help of insulin
- Glucose is stored as glycogen in our liver.
Whenever insulin levels drops, the stored glycogen is converted into glucose by liver to keep the glucose level within a normal range. Since there is no insulin or reduced levels of insulin in type 1 diabetes, the levels of sugar increases in bloodstream. This can result in life-threatening complications.
Various signs and symptoms associated with type 1 diabetes are:
- Increased thirst
- Recurrent urination
- Excessive hunger
- Loss of weight
- Exhaustion or tiredness
- Hazy vision
Risk Factors
Some of the known risk factors for type 1 diabetes include:
- Positive family history- Those with history of type 1 diabetes in a parent or sibling have higher chance of developing the disease
- Heredity- There is increased risk of developing type 1 diabetes in the presence of certain genes in body.
- Topography-The incidence of type 1 diabetes is two to three times higher in people living in certain geographical areas. Trend of disease is increased when we move away from equator.
- Contact with Virus- The autoimmune destruction of the islet cells can be triggered after exposure to epstein-barr virus, coxsackievirus, mumps virus or cytomegalovirus
It has been recommended by experts from international committee like the American Diabetes Association, the European Association for the Study of Diabetes and the International Diabetes Federation that testingfor type 1 diabetes include the:
- Glycatedhemoglobin (A1C) test. Patients average blood sugar level for the past three months can be detected by this test. If A1C level comes out to be of 6.5 percent or higher on two different tests ,this indicates that patient has diabetes.
- Random blood sugar test. In this test blood sample will be taken at a random time, regardless of time when you last ate. Blood sugar level of 200 mg/dL(11.1 mmol/L) or higher suggests diabetes, particularly when any of the signs and symptoms of diabetes are present.
- Fasting blood sugar test. Here blood sample is taken after an overnight fast. Fasting blood sugar value less than 100 mg/dL(5.6 mmol/L) is considered to be normal, while value from 100 to 125 mg/dL (5.6 to 6.9 mmol/L) is considered prediabetes. Fasting blood sugar value of 126 mg/dL (7 mmol /L) or higher on two separate tests is considered as having diabetes.
When patient is diagnosed to have diabetes, doctor may blood tests to check for auto antibodies that are common in type 1 diabetes.to differentiate between type 1 and type 2 diabetes.
Major organs of body like heart, blood vessels, nerves, eyes and kidneys are affected by type 1 diabetes. By keeping blood sugar levels under control one can considerably reduce the risk of developing the complications.
Type 1 diabetic patients develop long-term complications steadily over the years. Earlier the patient develops diabetes and the lesser the control of blood sugar levels, higher are chances of developing complications. Complications of diabetes can be disabling or even life-threatening.
- Heart and blood vessel disease. Diabetes increases risk of various cardiovascular diseases like chest pain (angina), heart attack, stroke, atherosclerosis-narrowing of arteries and high blood pressure.
- Damage to nerves (neuropathy). Diabetes can injure the walls of the tiny blood vessels (capillaries), especially in the legs. Symptoms of this are tingling, numbness, burning or pain that is usually first felt at the tips of the toes or fingers and slowly spreads upward. Uncontrolled blood sugar levels lead to loss ofl sense of feeling in the affected limbs. Damage to gastrointestinal tract nerves may cause problems like abdominal distention,alternate constipation and diarrhoea. Erectile dysfunction can occur in males.
- Damage to kidneys (nephropathy). Diabetes can damage filtering system of kidneys. Extensive injury can lead to kidney failure or irreversible end-stage kidney disease, which may lead to need for dialysis or a kidney transplant.
- Eye damage. Diabetes harm the blood vessels of the retina (diabetic retinopathy), leading to blindness. Diabetes can also result in other serious conditions, such as cataracts and glaucoma.
- Foot damage. Foot complications occur due to nerve damage in the feet or poor blood flow to the feet. Cuts and blisters in foot if left untreated can become serious infections. Sometimes toe, foot or even leg amputation may be required in severe damage.
- Skin and mouth conditions. Patients with diabetes are more prone to skin problems, including bacterial and fungal infections. Poor dental hygiene may lead to gum infections.
- Osteoporosis. Diabetes results in osteoporosis by lowering bone mineral density.
- Complications in pregnancy. Diabetes can increase risk of miscarriage, pregnancy-induced high blood pressure, preeclampsia stillbirth and birth defects.
Management of type 1 diabetes involves:
- Insulin
- Regular exercise
- Healthy food habits
- Blood sugar monitoring
Treatment aim is to keep blood sugar level as close to normal as possible to delay or prevent complications. Generally, the goal is to keep the premeals levels between 80 and 120 mg/dL (4.4 to 6.7 mmol/L) and 2hour postmeal levels between 100 and 160 mg/dL(5.6 to 7.8 mmol/L).However it is important to note that the target levels are absolutely individualized.
Insulin and other medications
Insulin is required by anyone who has type 1 diabetes. There are many types of insulin and include:
- Rapid-acting insulin
- Long-acting insulin
- Intermediate options
There is no method of taking Insulin orally and it has to be taken subcutaneously because stomach enzymes interfere with insulin's action.
Monitoring carbohydrates and healthy eating
There's no such thing as a diabetes diet, contrary to popular perception. There is no need to restrict the patient to a lifetime of boring, bland foods. Generally nutritious, low-fat, high-fiber foods such asFruits,Vegetables and Whole grains while restricting animal products and refined carbohydrates, such as white bread and sweets.
Physical activity
Regular aerobic exercise is needed by everyone, and people who have type 1 diabetes are no exception. Take approval from thedoctor to exercise. Find out activities that you enjoy, such as walking, swimming or biking. Do exercise routinely and aim for at least 30 minutes of aerobic exercise most days of the week. It is also important to do flexibility and strength training exercises.
Blood sugar monitoring
The patient may need to check and record theblood sugar level at least four times a day, and possibly more often depending on what type of insulin therapy is used — twice daily injections, multiple daily injections or insulin pump. The only way to make sure that the blood sugar level remains within the target range is by careful monitoring. The amount of sugar in the blood can change unpredictably in many situations.It is important to learn how the blood sugar level changes in response to:
- Food
- Physical activity
- Medication
- Illness
- Alcohol
- Stress
- For women, fluctuations in hormone levels
Type 2 Diabetes
Type 2 diabetes is also known as adult-onset or noninsulin-dependent diabetes. It is a chronic condition that affects the way the body metabolizes sugar (glucose), which is body's main source of fuel. In type 2 diabetes, body becomes resistant to the effects of insulin ( a hormone that enables the movement of sugar into cells) — or even may not produce enough insulin to sustain a normal glucose level. Type 2 diabetes if left untreated can be life-threatening.
Type 2 diabetes is common in adults but can also affect children. Type 2 diabetes is non curable but by eating well, exercising and maintaining a healthy weight we can manage the disease. If blood sugar is not controlled by diet and exercises, one may require diabetes medications or insulin therapy

When our body becomes resistant to the effect of insulin or when enough insulin is not produced by pancreas, one can develop type 2 diabetes. Why this happens is exactly not known, although obesity and physical inactivity seem to be causal factors.
The role of insulin
Insulin is one of the hormone that is secreted from the islets cells of pancreas, a gland to be found behind and below the stomach. When the islet cells are destroyed, there will be little or no insulin.
- Insulin is secreted from pancreas into the bloodstream.
- The circulating insulin helps sugar enter into cells
- Amount of sugar in ones bloodstream is lowered by insulin.
- Whenever blood sugar level drops, the secretion of insulin from pancreas also reduces.
The role of glucose
Glucose is a sugar which is one of the main sources of energy for the body cells that build up muscles and other tissues.
- Food and our liver are two main sources of glucose.
- Sugar from bloodstream enters inside the cells with the help of insulin
- Glucose is stored as glycogen in our liver.
Whenever insulin levels drops, the stored glycogen is converted into glucose by liver to keep the glucose level within a normal range. Since there is no insulin or reduced levels of insulin in type 1 diabetes, the levels of sugar increases in bloodstream. This can result in life-threatening complications.
Type 2 diabetes' symptoms develop slowly. Sometimes patient with have type 2 diabetes for years and not know it. Various symptoms are:
- Increased thirst and recurrent urination. Excess sugar building up in the bloodstream causes fluid to be pulled from the tissues. This may leave one thirsty. As a result, one may drink — and urinate — more than usual.
- Increased hunger. Without enough insulin to move sugar into the cells, the muscles and organs become depleted of energy. This triggers intense hunger.
- Weight loss. Despite eating more than usual to relieve hunger, one may lose weight. Without the ability to metabolize glucose, the body uses alternative fuels stored in muscle and fat. Calories are lost as excess glucose is released in the urine.
- Fatigue. If the cells are deprived of sugar, one may become tired and irritable.
- Blurred vision. If the blood sugar is too high, fluid may be pulled from the lenses of the eyes. This may affect the ability to focus clearly.
- Slow-healing sores or frequent infections. Type 2 diabetes affects the ability to heal and resist infections.
- Areas of darkened skin. Some people with type 2 diabetes have patches of dark, velvety skin in the folds and creases of their bodies — usually in the armpits and neck. This condition, called acanthosis nigricans, may be a sign of insulin resistance.
Risk Factors
Certain factors which increase the risk of developing type 2 diabetes include:
- Obesity. Obesity is a major risk factor for type 2 diabetes. The more body fat you have, the more resistant body cells become to insulin.
- Distribution of fat. If one have fat primarily in abdominal area, chances of type 2 diabetes is greater than when body stores fat elsewhere.
- Inactivity. The risk of type 2 diabetes is more in physically inactive persons. Physical activity helps in using up glucose as energy and makes cells more sensitive to insulin.
- Family history. Chances of type2diabetes are more in those whose parent or sibling has type 2 diabetes.
- Race. People of certain races — including blacks, Hispanics, American Indians and Asian-Americans — are more prone to develop type 2 diabetes than whites are.
- Age. The risk of type 2 diabetes is greater, especially after age 45. Type 2 diabetes is also increasing considerably among children, adolescents and younger adults.
- Prediabetes. Prediabetes is a condition where your blood sugar levels are higher than normal, but not high enough to be labeled as diabetes. Prediabetes if ignored often progresses to type 2 diabetes.
- Gestational diabetes. Females developing gestational diabetes during pregnancy are at risk of developing type 2 diabetes
The American Diabetes Association, the European Association for the Study of Diabetes and the International Diabetes Federation recommended that type 2 diabetes testing include the:
- Glycated hemoglobin (A1C) test. This blood test indicates THE average blood sugar level for the past two to three months. It works by measuring the percentage of blood sugar attached to hemoglobin, the oxygen-carrying protein in red blood cells. The higher THE blood sugar levels, the more hemoglobin you'll have with sugar attached. An A1C level of 6.5 percent or higher on two separate tests indicates you have diabetes.If the A1C test isn't available, or if you have certain conditions that can make the A1C test inaccurate — such as if you're pregnant or have an uncommon form of hemoglobin (known as a hemoglobin variant) — THE doctor may use the following tests to diagnose diabetes:
- Random blood sugar test. A blood sample will be taken at a random time. Regardless of when you last ate, a random blood sugar level of 200 mg/dL (11.1 mmol/L) or higher suggests diabetes, especially when coupled with any of the signs and symptoms of diabetes, such as frequent urination and extreme thirst.
- Fasting blood sugar test. A blood sample will be taken after an overnight fast. A fasting blood sugar level less than 100 mg/dL (5.6 mmol/L) is normal. A fasting blood sugar level from 100 to 125 mg/dL (5.6 to 6.9 mmol/L) is considered prediabetes. If it's 126 mg/dL (7 mmol/L) or higher on two separate tests, you have diabetes.
- Oral glucose tolerance test. This test is now rarely used, in this patient fast overnight, and the fasting blood sugar level is measured. Pt is then given a measured quantity of glucose and blood sugar levels are tested repeatedly for the next two hours. A blood sugar level less than 140 mg/dL (7.8 mmol/L) is normal. Blood sugar level more than 200 mg/dL (11.1 mmol/L) after two hours indicates diabetes and reading between 140 and 199 mg/dL (7.8 mmol/L and 11.0 mmol/L) indicates prediabetes.Routine screening for type 2 diabetes beginning at age 45, especially if one is overweight has been recommended by the American Diabetes Association. If the results are normal, repeat the test every three years. If the results are borderline, consult doctor when to come back for another test. Screening is also advised for people who are under 45 and overweight and /having other risk factors
Type 2 diabetes damages many major organs like heart, blood vessels, nerves, eyes and kidneys. These complications can be prevented by controlling blood sugar levels.
Since long-term complications of diabetes develop slowly but they can eventually be disabling or even life-threatening. Various complications of diabetes include:
- Cardiovascular disorder. Diabetes significantly increases the chances of various cardiovascular problems, including coronary artery disease with chest pain, heart attack, stroke, narrowing of arteries (atherosclerosis) and high blood pressure.
- Neuropathy-nerve damage. Type 2 diabetes can injure the walls of the tiny blood vessels (capillaries), especially in the legs. It results in tingling, lack of sensation, burning or pain that usually begins at the tips of the toes or fingers and slowly spreads upward. Uncontrolled blood sugar can result in complete loss of sensations in the affected limbs Damage to gastrointestinal tract nerves cause problems like sickness, vomiting, diarrhea or constipation. Erectile dysfunction can occur in males.
- Damage to kidneys (nephropathy). Diabetes can damage filtering system of kidneys. Extensive injury can lead to kidney failure or irreversible end-stage kidney disease, which may lead to need for dialysis or a kidney transplant.
- Eye damage. Diabetes harm the blood vessels of the retina (diabetic retinopathy), leading to blindness. Diabetes can also result in other serious conditions, such as cataracts and glaucoma.
- Foot damage. Foot complications occur due to nerve damage in the feet or poor blood flow to the feet Cuts and blisters in foot if left untreated can become serious infections. Sometimes toe, foot or even leg amputation may be required in severe damage..
- Skin and mouth conditions. Patients with diabetes become prone to skin problems, including bacterial and fungal infections. Poor dental hygiene may lead to gum infections
- Osteoporosis. Diabetes results in osteoporosis by lowering bone mineral density.
- Alzheimer's disease. The risk of Alzheimer's disease and vascular dementia is increased in type 2 diabetes.
For effective management of type 2 diabetes it requires a lifelong assurance to:
- Blood sugar monitoring
- Healthy eating
- Regular exercise
- Regular medication or insulin therapy
These steps will help keep the blood sugar level closer to normal.
Diabetes medications
Newly diagnosed patients will be prescribed metformin, a diabetes medication that improves your body tissues' sensitivity to insulin and lowers glucose production in the liver. Your doctor will also recommend lifestyle changes, such as losing weight and becoming more active.
After some time, metformin is not enough to control the glucose level. It is the time to add other oral or injected medications. Medications lower glucose in different ways. Some diabetes medications stimulate the pancreas to produce and release more insulin. They include glipizide, glyburide and glimepiride. Still others block the action of enzymes that break down carbohydrates in the intestine, such as acarbose, or make the tissues more sensitive to insulin, such as metformin or pioglitazone.Some other oral drugs are:
- Sitagliptin
- Saxagliptin
- Repaglinide
- Nateglinide
Recently approved drugs given by injection are:
- Exenatide
- Liraglutide
Additionally, the doctor might prescribe low-dose aspirin therapy as well as blood pressure and cholesterol-lowering medications to help prevent heart and blood vessel disease.
Insulin therapy
Some type 2 diabetics may need insulin therapy as well. Because normal digestion interferes with insulin taken by mouth, insulin must be injected. Insulin injections involve using a fine needle and syringe or an insulin pen injector — a device that looks like an ink pen, except the cartridge is filled with insulin.
Bariatric surgery
In obese diabetics, weight-loss surgery (bariatric surgery) is advised to reduce body fat. Blood sugar levels return to normal in 55 to 95 percent of people with diabetes, depending on the procedure performed.
Pregnancy
During pregnancy, women with type 2 diabetes will likely need to alter their treatment. During pregnancy, you'll likely be switched to insulin therapy. Also, many blood pressure and cholesterol-lowering medications can't be used during pregnancy.
Signs of trouble
Problems can arise because so many factors can affect your blood sugar
- High blood sugar (hyperglycemia).
- Increased ketones in your urine (diabetic ketoacidosis).
- Hyperglycemic hyperosmolar nonketotic syndrome (HHNS).
- Low blood sugar (hypoglycemia).
Blood sugar levels should be checked regularly, and patients should watch for signs and symptoms of low blood sugar — sweating, shakiness, weakness, hunger, dizziness, headache, blurred vision, heart palpitations, slurred speech, drowsiness, confusion and seizures.
Prevention
Diabetes can be prevented by healthy lifestyle choices
- Eat healthy foods.
- Get regular physical exercise.
- Lose excess weight.
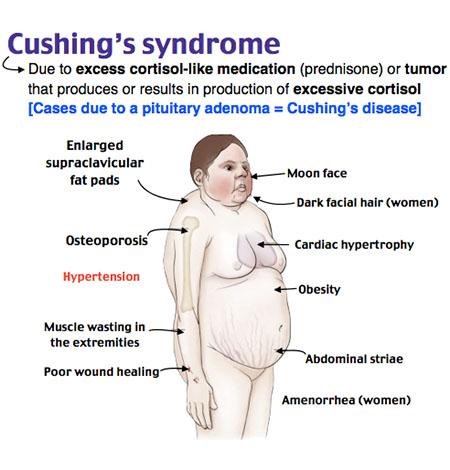
Cushing's syndrome
When the body is exposed to high levels of the hormone cortisol for a long time it is called Cushing syndrome which can be because the body is making too much of cortisol or by the use of excess oral corticosteroid medication
An excess of cortisol can produce some of the hallmark signs of Cushing syndrome — a fatty hump between the shoulders, a rounded face, and pink or purple stretch marks on the skin. Cushing syndrome can also result in high blood pressure, bone loss and diabetes.
There are a number of reasons for Cushing syndrome and these include the following:
Pituitary adenoma - Cushings disease
Adenoma of the pituitary is a small, benign (non-cancerous) tumor in the pituitary. It is usually less than 1 cm in size, and is made of abnormal cells which make lots of ACTH. The ACTH stimulates the adrenals which then make too much cortisol. About 4 in 5 cases of Cushing's syndrome are caused by a pituitary adenoma .Cushing's syndrome caused by a pituitary adenoma is called Cushing's disease.
Adrenal problems
Various rare disorders of the adrenal glands exist which can cause high levels of cortisol. These include:
- Adrenal hyperplasia. In this disorder there is increased number and growth of the cells in the adrenal glands. These cells then make too much cortisol. There are various different types of adrenal hyperplasia.
- Non-cancerous tumor of an adrenal gland.
- Cancerous tumor of an adrenal gland (very rare).
Other causes of too much ACTH ('ectopic ACTH')
In many cases, some rare tumors in other parts of the body make ACTH - for example, some types of lung cancer. The ectopic ACTH (that is, ACTH not made in the pituitary) then stimulates the adrenal glands to make too much cortisol. A variety of tumors can make ACTH, some malignant, and some benign (non-cancerous). Some benign tumors are so small that it is very difficult to find where in the body the excess ACTH is being made.
Steroid medicines
Steroid medications similar to cortisol are prescribed to some people to treat some disorders. This is sometimes used to treat various conditions such as some types of arthritis, and for some cancers. Long-term treatment with steroids can cause symptoms and problems similar to Cushing's syndrome.
Other causes
- People who drink too much alcohol make too much cortisol. The cortisol level goes back to normal if drinking alcohol stops.
- People with severe depression also make too much cortisol.
There is a variation in signs and symptoms of Cushing syndrome. Common signs and symptoms involve progressive obesity and skin changes, such as:
- Excessive gain in weight and fatty tissue deposits, particularly around the midsection and upper back, in the face (moon face), and between the shoulders (buffalo hump)
- Stretch marks that are pink or purple (striae) colored and present on the skin of the abdomen, thighs, breasts and arms
- Thinning, fragile skin that bruises easily
- Delayed healing of cuts, insect bites and infections
- Facial acne
In women with Cushing syndrome, the symptoms could include:
- Thicker or more visible body and facial hair (hirsutism)
- Irregular or absent menstrual periods
In men with Cushing syndrome, symptoms could include:
- Reduced libido
- Reduced fertility
- Erectile dysfunction
Other signs and symptoms include:
- Generalized fatigue
- Generalized muscle weakness
- Depression, anxiety and irritability
- Lack of emotional control
- Difficulties in cognition
- New or worsened high blood pressure
- Glucose intolerance that may lead to diabetes
- Headache
- Loss of bone, leading to fractures over time
It is difficult to diagnose Cushing syndrome, particularly endogenous Cushing syndrome, because other conditions share the same signs and symptoms. It will be required to conduct a physical exam, to look for signs of Cushing syndrome. Cushing syndrome if there is signs such as rounding of the face (moon face), a pad of fatty tissue between the shoulders and neck (buffalo hump), and thin skin with bruises and stretch marks.
Patients on a corticosteroid medication for a long time may be suspected of developing Cushing syndrome as a result of this medication. If there is no history of using a corticosteroid medication, these diagnostic tests may help pinpoint the cause:
- Blood and urine tests. Doctors conduct these tests to measure hormone levels in the urine and blood and show whether the body is producing excessive cortisol. For the urine test, you may be asked to collect the urine over a 24-hour period. Both the urine and blood samples will be sent to a laboratory to be analyzed for cortisol levels.
- Other specialized tests. Tests that evaluate the blood and urine may help to determine if Cushing syndrome is present and to help identify the underlying source of any excess production. These tests often involve measuring cortisol levels before and after stimulation or suppression with other hormone medications.
- Imaging tests. Images of the pituitary and adrenal glands to detect abnormalities, such as tumors, can be provided by computerized tomography scans or magnetic resonance imaging scans.
Cushing syndrome management aims to lower the high level of cortisol in the body. The best treatment for you depends on the cause of the syndrome. Treatment options include:
- Decreasing corticosteroid use. The doctor may be able to keep the Cushing signs and symptoms under control, if they are caused by long-term use of corticosteroids, by reducing the dosage of the drug over a period of time, while still adequately managing the asthma, arthritis or other condition for which it was given
- Surgery. The doctor may recommend complete surgical removal if the cause of Cushing syndrome is a tumor. Pituitary tumors are typically removed by a neurosurgeon. If a tumor is present in the adrenal glands, lungs or pancreas, the surgeon can remove it through a standard operation or in some cases by using minimally invasive surgical techniques, with smaller incisions. You'll need to take cortisol replacement medications after the operation to provide the body with the correct amount of cortisol. You'll eventually experience a return of normal adrenal hormone production, in most cases, and the doctor can taper off the replacement drugs. However, this process can take up to a year or longer. In some instances, people with Cushing syndrome never experience a resumption of normal adrenal function; they then need lifelong replacement therapy.
- Radiation therapy. In case surgery is unable to totally remove the pituitary tumor, doctor will usually prescribe radiation therapy to be used in conjunction with the operation. Additionally, radiation may be used for people who aren't suitable candidates for surgery. Radiation can be given in small doses over a six-week period or by a technique called stereotactic radiosurgery (Gamma Knife surgery). In the latter procedure, administered as a single treatment, a large dose of radiation is delivered to the tumor, and the radiation exposure to surrounding tissues is minimized.
- Medications. When surgery and radiation don't work medications can be used to control cortisol production. Medications may also be used before surgery in people who have become very sick with Cushing syndrome. Doctors recommend drug therapy before surgery to improve signs and symptoms and minimize surgical risk.
Gestational Diabetes
Diabetes that makes its appearance for the first time during pregnancy is classified under gestational diabetes. Like other types of diabetes, gestational diabetes is characterized by high levels of blood sugar in the body due to the inability of insulin to push the glucose present in the blood into the cells.
Blood sugar usually returns to normal soon after delivery in gestational diabetes in the majority but it may persist too.Gestational dIabetes places the patients at risk for type 2 diabetes.

It is not known how and why some women develop gestational diabetes. To understand how gestational diabetes occurs, it can help to understand how pregnancy affects the body's normal processing of glucose.
The food eaten is digested by the body to produce sugar (glucose) that enters the bloodstream. In response, the pancreas — a large gland behind the stomach — produces insulin. Insulin is a hormone that helps glucose move from the bloodstream into the body's cells, where it's used as energy.
The placenta that connects the growing baby to the blood supply produces high levels of various other hormones during pregnancy. Almost all of them impair the action of insulin in the cells, raising the blood sugar. Modest elevation of blood sugar after meals is normal during pregnancy.
The placenta produces more and more insulin-blocking hormones as pregnancy progresses. In gestational diabetes, the placental hormones provoke a rise in blood sugar to a level that can affect the growth and welfare of the baby. Gestational diabetes usually develops during the last half of pregnancy — sometimes as early as the 20th week.
Risk factors
Gestational diabetes can develop in any female, but some women are at greater risk. Risk factors for gestational diabetes include:
- Greater than 25 age. Women older than age 25 are more likely to develop gestational diabetes.
- Personal or family health history. The risk of developing gestational diabetes increases if you have prediabetes — slightly elevated blood sugar that may be a precursor to type 2 diabetes — or if a close family member, such as a parent or sibling, has type 2 diabetes. You're also more likely to develop gestational diabetes if you had it during a previous pregnancy, if you delivered a baby who weighed more than 9 pounds (4.1 kilograms), or if you had an unexplained stillbirth.
- Being overweight. You're more likely to develop gestational diabetes if you're significantly overweight with a body mass index (BMI) of 30 or higher.
- Racial factors. For reasons that aren't clear, women who are black, Hispanic, American Indian or Asian are more likely to develop gestational diabetes.
Gestational diabetes, for most women doesn't cause noticeable signs or symptoms. Rarely, gestational diabetes may cause excessive thirst or increased urination.
Seek health care early, if possible, when you first think about trying to get pregnant — so the doctor can evaluate the risk of gestational diabetes as part of the overall childbearing wellness plan. Once you become pregnant, the doctor will address gestational diabetes as part of the regular prenatal care. If you develop gestational diabetes, you may need more frequent checkups. These are most likely to occur during the last three months of pregnancy, when the doctor will carefully monitor the blood sugar level and the baby's health.
You may be referred to additional health professionals who specialize in diabetes management, such as an endocrinologist, a registered dietitian or a diabetes educator. They can help you learn to manage the blood sugar level during the pregnancy.
The health care team will check the blood sugar right after delivery and again in six weeks to make sure that the blood sugar level has returned to normal after the baby is born. Once you've had gestational diabetes, it's a good idea to have the blood sugar level tested regularly. The frequency of blood sugar tests will in part depend on the test results soon after you deliver the baby.
There is no single set of screening guidelines for gestational diabetes. Some question whether gestational diabetes screening is needed if you're younger than 25 and have no risk factors. Others say that screening all pregnant women — no matter their age — is the best way to catch all cases of gestational diabetes.
When to screen
Evaluation of the risk factors by the doctor will happen for gestational diabetes early in the pregnancy.
In case of a higher risk— for example, the body mass index (BMI) before pregnancy was 30 or higher or you have a mother, father, sibling or child with diabetes — the doctor may test for diabetes at the first prenatal visit. You'll likely have a screening test for gestational diabetes sometime during the second trimester — between 24 and 28 weeks of pregnancy if you're at average risk of gestational diabetes.
Routine screening for gestational diabetes
Glucose challenge test (initial). This tests begins by drinking a syrupy glucose solution. One hour later, you'll have a blood test to measure the blood sugar level. A blood sugar level below 130 to 140 milligrams per deciliter (mg/dL), or 7.2 to 7.8 millimoles per liter (mmol/L), is usually considered normal on a glucose challenge test, although this may vary at specific clinics or labs. If the blood sugar level is higher than normal, it only means you have a higher risk of gestational diabetes. The doctor will diagnose you after giving you a follow-up test.
Glucose tolerance testing (follow up). You'll be asked to fast overnight for the follow-up test and then have the fasting blood sugar level measured. Then you'll drink another sweet solution — this one containing a higher concentration of glucose — and the blood sugar level will be checked every hour for a period of three hours. If at least two of the blood sugar readings are higher than normal, you'll be diagnosed with gestational diabetes.
If you're diagnosed with gestational diabetes
The doctor will likely recommend frequent checkups if you have gestational diabetes, especially during the last three months of pregnancy. During these exams, the doctor will carefully monitor the blood sugar. The doctor may also ask you to monitor the own blood sugar daily as part of the treatment plan.
You may need additional tests to evaluate the baby's general health if you're having trouble controlling the blood sugar, or you need to take insulin, or you have other pregnancy complications.
Monitor and control the blood sugar to keep the baby healthy and avoid complications during the pregnancy and delivery. Also keep a close eye on the future blood sugar levels. Management strategies may include:
- Blood sugar monitoring. The health care team may ask you to check the blood sugar four to five times a day while you're pregnant — first thing in the morning and after meals — to make sure the level stays within a healthy range. This may sound inconvenient and difficult, but it'll get easier with practice.
Blood sugar monitoring will also be done during labor and delivery. Follow-up blood sugar checks are also important. After having gestational diabetes, you're at increased risk of later developing type 2 diabetes. Work with the health care team to keep an eye on the levels. Maintaining health-promoting lifestyle habits, such as a healthy diet and regular exercise, can help reduce the risk. - Healthy diet. The best way to control blood sugar is to eat the right kinds and quantity of food. Doctors don't advise losing weight during pregnancy — the body is working hard to support the growing baby. But the doctor can help you set weight gain goals based on the weight before pregnancy. Making healthy food choices can help prevent excessive weight gain, which can put you at higher risk of complications.
A healthy diet often focuses on fruits, vegetables and whole grains — foods that are high in nutrition and fiber and low in fat and calories — and limits highly refined carbohydrates, including sweets. - Regular exercise. Physical activity plays a key role in every woman's wellness plan before, during and after pregnancy. Exercise lowers the blood sugar by stimulating the body to move glucose into the cells, where it's used for energy. Exercise also increases the cells' sensitivity to insulin, which means the body produces less insulin to transport sugar. Aim for moderately vigorous exercise on most days of the week.
- You may need insulin injections to lower the blood sugar if diet and exercise aren't enough. Between 10 and 20 percent of women with gestational diabetes need insulin to reach their blood sugar goals. Some doctors may prescribe an oral blood sugar control medication, such as metformin.
- Baby's close monitoring. Close observation of the baby is an important part of the treatment plan.
Gigantism & Acromegaly
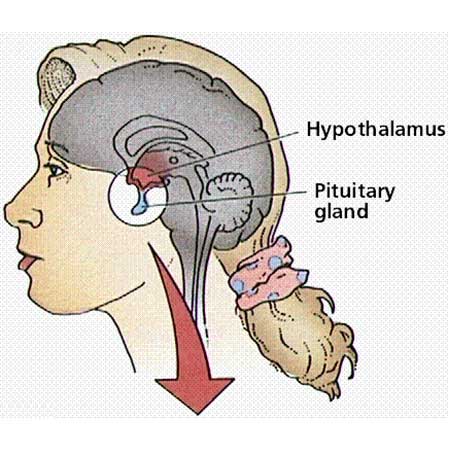
Acromegaly, also called as gigantism, is a rare disease in which you make too much growth hormone. Due to this there are various symptoms which slowly develop over several years. Common symptoms are that the hands and feet become larger, and features of the face may become more prominent. The cause is usually a small non-cancerous tumor in the pituitary gland. The pituitary gland lies just below the brain. Pituitary hormone produces several hormones, including growth hormone. Hormone secreted by the body is partly controlled by other hormones which come from a small part of the brain called the hypothalamus. This is just above the pituitary.It makes growth hormone-releasing hormone (GHRH) which stimulates the pituitary to make growth hormone when the blood level of growth hormone is low. It also makes a hormone called somatostatin which prevents the pituitary from making growth hormone when the level of growth hormone is high.
Growth hormone helps to stimulate growth and repair of various body tissues. It is needed in childhood to help children to grow. Growth hormone acts on some tissues directly.
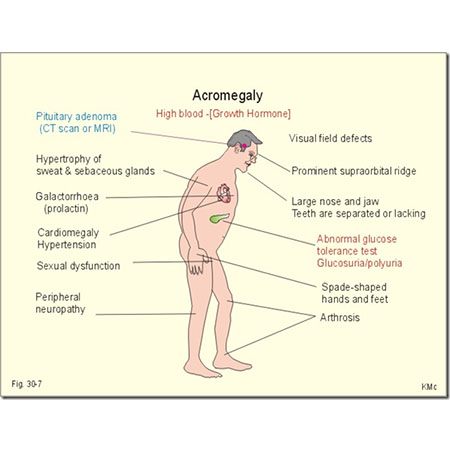
The cause of acromegaly is pituitary gland overproducing growth hormone (GH) over time. Secretion of GH into the bloodstream triggers the liver to produce a hormone called insulin-like growth factor-I (IGF-I). Excess of IGF-I can cause abnormal growth of the soft tissues and skeleton and other signs and symptoms characteristic of acromegaly and gigantism.
A tumor is the most common cause of too much GH production in adults:
- Tumors of Pituitary. Majority of acromegaly cases are caused by a noncancerous (benign) tumor (adenoma) of the pituitary gland. The tumor secretes excessive amounts of growth hormone, causing many of the signs and symptoms of acromegaly. Some of the symptoms of acromegaly, such as headaches and impaired vision, are due to the tumor mass pressing on nearby brain tissues.
- Tumors from other sites. Tumors in other parts of the body, such as the lungs, pancreas or adrenal glands, cause the disorder in a few people with acromegaly. Sometimes, these tumors actually secrete GH. In other cases, the tumors produce a hormone called growth hormone-releasing hormone (GH-RH), which stimulates the pituitary to make more GH.
The literal meaning of acromegaly is 'enlarged extremities' or 'enlarged hands and feet'. This is a typical feature, but there are many other symptoms. The symptoms develop gradually. Some people have symptoms which develop over 10-15 years before the diagnosis is made.The symptoms are divided into two types: those caused by too much growth hormone, and those caused by the enlarging tumor (adenoma) in the pituitary.
Symptoms caused by too much growth hormone
GH excess in the bloodstream can affect various tissues in the body which can make them thicken or grow. Most patients develop following symptoms:
- Large and broad hands and feet. The glove and shoe size may increase over the years. You may not be able to get a wedding ring off.
- The skin may thicken (particularly on the face) and become more greasy and sweaty.
- Face changes may include: thickened lips and nose, thickening of the scalp, the jaw becoming more prominent. These changes develop very gradually so may not actually be noticed by the family or friends. However, looking back at old photographs may suggest the facial appearance has changed.
- Thickening of vocal cords which may cause the voice to deepen.
- The tongue may enlarge so you may often bite the tongue.
- Thickening of cartilage may cause arthritis in various joints.
- Nasal passage thickening can make you snore loudly and may cause obstruction in airflow when you are asleep (sleep apnoea). This can make you have a poor night's sleep with daytime drowsiness.
- Carpal tunnel syndrome. This is where a nerve going through the wrist is squashed by thickened tissue. It can cause pain, tingling and weakness in parts of the hands or arms.
- Irregular or absent periods (in women) may occur.
Other symptoms may include:
- Tiredness in general.
- Muscle weakness.
- About 1 in 5 people with acromegaly also develop diabetes as growth hormone counters the effects of insulin.
- Raised blood pressure develops in about 1 in 3 cases.
- Raised risk of heart disease and stroke. This is probably because of the increased risk of developing high blood pressure and diabetes.
- increased chance of developing polyps (small benign growths) in the bowel and a slightly increased chance of developing bowel cancer. People with acromegaly are now routinely screened for these conditions.
Symptoms caused by the growing tumor
Tumor, in many cases, remains small and does not cause pressure symptoms. However, in some cases the tumor grows enough to cause pressure on the nearby tissues. This can lead to:
- Headaches.
- Vision problems. The tumor may press on the optic nerves (the nerves going from the eyes to the brain) which are just next to the pituitary.
- Other normal cells in the pituitary may become squashed and damaged. Therefore, you may develop a lack of other hormones that are made by the pituitary. This can cause an underactive thyroid gland and/or an underactive adrenal gland which can cause various other symptoms.
- Blood test can measure the level of growth hormone. However, a single test is not reliable. This is because the levels of growth hormone in the body fluctuate a lot throughout the day in all people.
- Acromegaly diagnosis can also be made by a glucose tolerance test. In this test you drink a sugar drink containing 75 grams of glucose. You then have a series of blood tests over two hours. The glucose should lower the blood level of growth hormone. However, if you have acromegaly the growth hormone level remains high.
- Blood test may measure the level of IGF-1 if acromegaly is suspected. This may also be used as an index of disease activity to assess how well treatment is working.
- Magnetic resonance imaging (MRI) scan can show the size of any tumor.
- Eye and visual tests can assess if the tumor is pressing on the optic nerve.
- If you are confirmed as having acromegaly, other tests will be needed to see if the tumor is causing a lack or excess of other hormones made by the pituitary.
- Other tests may include chest X-ray, electrocardiogram (ECG) and X-rays of some of the joints
Common complications of acromegaly are:
- • High blood pressure (hypertension)
- • Cardiovascular disease, particularly enlargement of the heart (cardiomyopathy)
- Osteoarthritis
- Diabetes mellitus
- Precancerous growths (polyps) on the lining of the colon
- Sleep apnea, a condition in which breathing repeatedly stops and starts during sleep
- Carpal tunnel syndrome
- Reduced secretion of other pituitary hormones (hypopituitarism)
- Uterine fibroids, benign tumors in the uterus
- Spinal cord compression
- Vision los
Management goal in acromegaly is to reduce the level of growth hormone in the blood to normal, and to reduce the size of an enlarged tumor. Many of the symptoms and features of acromegaly will reverse or improve with successful treatment (apart from any fixed extra bone growth that had occurred).
Surgery
The most common treatment is to remove the adenoma by surgery. This is done using very fine instruments. Doctors can remove most pituitary tumors using a method called transsphenoidal surgery. In this procedure, the surgeon works through the nose to extract the pituitary tumor. Removing the tumor can normalize GH production and eliminate the pressure on the tissues surrounding the pituitary to relieve associated signs and symptoms. In some cases, the surgeon may not be able to remove the entire tumor. This may result in persistently elevated GH levels after surgery, requiring further medical or radiation treatments.
Medicine
Somatostatin analogues (octreotide and lanreotide).
These medications reduce the level of growth hormone to normal in over half of cases, and reduce the size of the tumor in about 8 in 10 cases. However, these medicines need to be given as an injection. They work in a similar way to somatostatin which is a hormone that prevents growth hormone from being released from pituitary cells. These medicines used to be injected several times a day. However, longer-acting preparations are now available as monthly or fortnightly injections. Side-effects are not common with these medicines. Some people develop abdominal pains and diarrhea, but these usually wear off with time. Gallstones can also occur but rarely cause problems.
Dopamine agonists (such as cabergoline, bromocriptine and quinagolide).
These medications can be taken as tablets. They work by preventing the release of growth hormone from tumor cells. However, they only work well in about 1 in 5 cases. Side-effects such as feeling sick and dizzy are also quite common.
Pegvisomant.
This medication is taken as a daily injection. However, unlike the other medicines listed above, it does not act directly at the pituitary. Pegvisomant works by blocking the action of growth hormone on the body's cells. Therefore, although many of the symptoms of growth hormone excess will be eased, it does not reduce the size of the tumor and headaches are not eased.
Radiotherapy
Therapy with radiation is an option to reduce the size of the tumor and hence reduce the production of growth hormone. Radiotherapy focuses high-intensity radiation at the pituitary tumor to destroy the abnormal cells. It may be used if you are not able to have surgery, or if surgery was only partially successful. However, it can take months or years after the radiotherapy is given for the level of growth hormone to reduce to normal. You can take medication whilst waiting for the effects of radiotherapy to work.
A possible side-effect of pituitary radiotherapy is damage to other normal pituitary cells. This can cause a reduced level of some other hormones.
Prolactinoma & Hyperprolactinaemia
Noncancerous tumor (adenoma) of the pituitary gland in the brain is called prolactinoma. It overproduces the hormone prolactin which is called as hyperprolactinaemia. The major effect of increased prolactin is a decrease in levels of some sex hormones — estrogen in women and testosterone in men. Prolactinoma can impair the vision, cause infertility and produce other effects, although it isn't life-threatening.
Medications can often restore the prolactin level to normal and helping in treating prolactinoma. Surgery to remove the pituitary tumor also may be an option to treat prolactinoma.
These are tumors that develops in the pituitary gland. The cause of these tumors remains unknown.
A small bean-shaped gland situated at the base of the brain is called the pituitary gland. Despite its small size, the pituitary gland influences nearly every part of the body. Its hormones one of which is prolactin, help regulate important functions such as reproduction.
Prolactin overproduction can be due to medications, other types of pituitary tumors, an underactive thyroid gland, an injury to the chest, pregnancy and breast-feeding.
Increased level of prolactin in the blood can cause various symptoms. The symptoms differ slightly between men, women and children. Symptoms in women may include:
- Irregularity of periods or no periods.
- Reduction in fertility.
- Reduction in sex drive.
- Leaking of milk from the breasts (known as galactorrhoea). The milk may leak out by itself, or may only show when the breast is squeezed.
- Rapid growth of hair on the face or body.
Symptoms in men may include:
- Reduction in fertility.
- Erectile dysfunction (difficulty having an erection).
- Decreased libido (reduced sex drive).
- Enlargement of breast (called gynaecomastia).
- Leakage of milk from the breasts.
Symptoms in children and teenagers may include:
- Delay in puberty.
Large prolactinomas may press on the brain or nearby nerves (the nearest nerves are the optic nerves which go to the eye). This may cause symptoms such as: - Headache.
- Symptoms with vision - you may get reduced vision or double vision. The early changes can easily go unnoticed, because they affect the peripheral vision - that is, the edges of the vision to the extreme left and right. This means that you may see less of what is around you, but can still see well if you focus on something directly.
See a doctor urgently if you have headaches or reduced vision - you may need to have treatment promptly to relieve the pressure on the optic nerves. The prolactinoma, rarely, may press on the rest of the pituitary gland, stopping it from producing other hormones.
Symptoms can suggest diagnosis. Women tend to be diagnosed earlier than men, because a change in the woman's periods is an early symptom and is easily noticed. Some prolactinomas are diagnosed by chance, if you have tests for another reason. If a prolactinoma is suspected, you may be offered several tests.
Blood tests
Level of prolactin can be checked in. If a high prolactin level is found, you may be asked to have a repeat test. This is because prolactin levels can be affected by many other things in the body, such as sleep or stress. It may help to take the blood sample when you are reasonably rested and have been awake for at least two hours.
Prolactin levels can range greatly and the normal level of prolactin is less than 400 mU/l. A very high prolactin level (>5000 mU/l) usually means that a prolactinoma is present. Levels in between may be due to a prolactinoma, or to other causes.
At the same time, other blood tests may be done. It is important to test the thyroid gland and to check kidney function, as both these can affect prolactin levels. Further tests may be needed to see if the tumour is causing a lack of other hormones made by the pituitary.
Eye tests
These tests will evaluate if the tumour is pressing on the optic nerve - this includes a test of visual fields.
Scans
Size of the tumor can be evaluated by a magnetic resonance imaging (MRI) scan or a computed tomography (CT) scan. A bone density scan may be advised for some patients, to check whether you are at risk of osteoporosis (which is a possible complication - see below)
Prolactinoma can have complications which may include:
- • Loss of vision. Left untreated, a prolactinoma may grow large enough to compress the optic nerve.
- • Hypopituitarism. Pressure on the normal pituitary gland, with larger prolactinomas, can cause dysfunction of other hormones controlled by the pituitary, resulting in hypothyroidism, adrenal insufficiency and growth hormone deficiency.
- • Loss of bone loss (osteoporosis). Too much prolactin can reduce production of the hormones estrogen and testosterone, resulting in decreased bone density and an increased risk of osteoporosis.
Goals of treatment are:
- Reduce the production of prolactin to normal levels
- Normal pituitary gland function restoration
- Galactorrhea elimination
- Reduction in the size of the pituitary tumor
- Abolish any signs or symptoms from tumor pressure, such as headaches or vision problems
Treatment of prolactinoma consists of two main therapies, medications and surgery:
Medications
Drugs given by mouth often can decrease the production of prolactin and eliminate symptoms. Medications may also shrink the tumor. However, long-term treatment with medications is generally necessary.
Known drugs such as dopamine agonists can be used to treat prolactinoma. These drugs mimic the effects of dopamine — the brain chemical that normally controls prolactin production — but are much more potent and long lasting. Commonly prescribed medications include bromocriptine (Cycloset, Parlodel) and cabergoline. These drugs decrease prolactin production and may shrink the tumor in most people with prolactinoma.
The common side effects of these drugs are lightheadedness, nausea and nasal stuffiness are common side effects of these medications. However, these side effects often can be minimized if the doctor starts you with a very low dose of medication and gradually increases the dose. Cabergoline has less frequent and less severe side effects, but it's more expensive than bromocriptine and newer, so its long-term safety record isn't as well established. There have been rare cases of heart valve damage with cabergoline. Some people may also develop compulsive behaviors, such as gambling, while taking these medications.
You may be able to eventually stop taking the medication if medication effectively shrinks the tumor and the prolactin level remains normal for two years afterward,. The doctor can offer you advice on when this may be possible for you. However, don't stop taking either drug without the doctor's approval.
Surgery
Surgery may be an option for the removal of a pituitary tumor if drug therapy for the treatment of prolactinoma doesn't work or you can't tolerate the medication. It may also be necessary to relieve pressure on the nerves that control the vision.
The size and extent of the tumor determines the type of surgery you require:
Surgery outcomes largely depend on the size and location of the tumor and the prolactin levels before surgery. The higher the prolactin level, the slimmer the chance that the prolactin production will return to normal after surgery. Surgery corrects the prolactin level in most people with small pituitary tumors. However, many pituitary tumors come back within five years of surgery. For people with larger tumors that can only be partially removed, drug therapy often can return the prolactin level to a normal range after surgery.
Radiation
Radiation therapy may be an option for people who don't respond to medication and aren't candidates for surgery.
Hyperthyroidism
The thyroid is a butterfly-shaped gland situated at the base of the neck, just below the Adam's apple. Although it weighs less than an ounce, the thyroid gland has an enormous impact on the health. Every aspect of the metabolism is regulated by thyroid hormones.
Thyroxine hormone has two type, thyroxine (T-4) and triiodothyronine (T-3), that influence almost every cell in the body. They maintain the rate at which the body uses fats and carbohydrates, help control the body temperature, influence the heart rate, and help regulate the production of protein. The thyroid also produces calcitonin, a hormone that helps regulate the amount of calcium in the blood.
A raised level of thyroid hormone is called as hyperthyroidism. It has various causes but Graves' disease is the most common cause. Hyperthyroidism can produce various symptoms. In an overactive thyroid gland, the thyroid gland makes too much thyroxine.
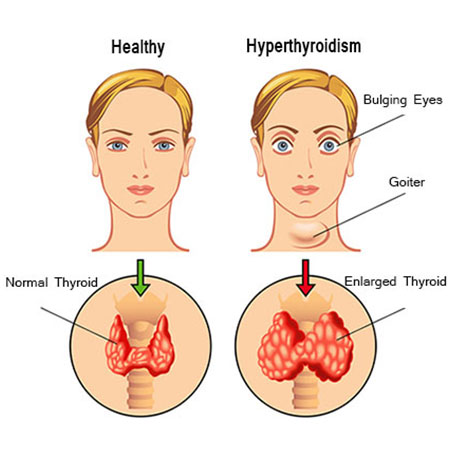
Many conditions can cause hyperthyroidism, including Graves' disease, toxic adenoma, Plummer's disease (toxic multinodular goiter) and thyroiditis.
Too much thyroxine (T-4) can be released due to many reasons, including:
- Graves' disease. It is an autoimmune disorder in which antibodies produced by the immune system stimulate the thyroid to produce too much T-4 It is the most common cause of hyperthyroidism. Normally, the immune system uses antibodies to help protect against viruses, bacteria and other foreign substances that invade the body. In Graves' disease, antibodies mistakenly attack the thyroid and occasionally attack the tissue behind the eyes (Graves' ophthalmopathy) and the skin, often in the lower legs over the shins (Graves' dermopathy).
- Hyperfunctioning thyroid nodules (toxic adenoma, toxic multinodular goiter, Plummer's disease). Hyperthyroidism of this form occurs when one or more adenomas of the thyroid produce too much T-4. An adenoma is a part of the gland that has walled itself off from the rest of the gland, forming noncancerous (benign) lumps that may cause an enlargement of the thyroid. Not all adenomas produce excess T-4, and doctors aren't sure what causes some to begin producing too much hormone.
- Thyroiditis. Inflammation of thyroid gland can result in hyperthyroidism. The inflammation can cause excess thyroid hormone stored in the gland to leak into the bloodstream. One type of thyroiditis, known as subacute thyroiditis, causes pain in the thyroid gland. Other types are painless and may sometimes occur after pregnancy (postpartum thyroiditis).
Many other disorders can be mimicked by hyperthyroidism, which may make it difficult for the doctor to diagnose. It can also cause a wide variety of signs and symptoms, including:
- Weight loss even when the appetite and the amount and type of food one eat remain the same or even increase
- Accelerated heartbeat (tachycardia) — commonly more than 100 beats a minute — irregular heartbeat (arrhythmia) or pounding of the heart (palpitations)
- Increased appetite
- Nervousness, anxiety and irritability
- Tremor — usually a fine trembling in the hands and fingers
- Sweating
- Changes in menstrual patterns
- Increased sensitivity to heat
- Changes in bowel patterns, especially more frequent bowel movements
- An enlarged thyroid gland (goiter), which may appear as a swelling at the base of the neck
- Fatigue, muscle weakness
- Difficulty sleeping
- Skin thinning
- Fine, brittle hair
Aged people are more likely to have either no signs or symptoms or subtle ones, such as an increased heart rate, heat intolerance and a tendency to become tired during ordinary activities.
Graves' ophthalmopathy
Rarely, Graves' ophthalmopathy may affect the eyes, especially if one smoke. It is a rare disorder In this disorder, the eyeballs protrude beyond their normal protective orbits when the tissues and muscles behind the eyes swell. This pushes the eyeballs forward so far that they actually bulge out of their orbits. This can cause the front surface of the eyeballs to become very dry. Eye problems often improve without treatment.
Graves' ophthalmopathy presents with:
- Protruding eyeballs
- Red or swollen eyes
- Excessive tearing or discomfort in one or both eyes
- Light sensitivity, blurry or double vision, inflammation, or reduced eye movement
Hyperthyroidism can be diagnosed by a simple blood test. A normal blood test will also rule it out if symptoms suggest that it may be a possible diagnosis. One or both of the following may be measured in a blood sample:
- Thyroid-stimulating hormone (TSH). Pituitary manufactures this hormone. It is released into the bloodstream. It stimulates the thyroid gland to make thyroxine. If the level of thyroxine in the blood is high, then the pituitary releases less TSH. Therefore, a low level of TSH means that the thyroid gland is overactive and is making too much thyroxine.
- Thyroxine (T4). A high level of T4 confirms hyperthyroidism.
Complications associated with hyperthyroidism include:
- Cardiovascular problems. Some of the most serious complications of hyperthyroidism involve the heart. These include a rapid heart rate, a heart rhythm disorder called atrial fibrillation and congestive heart failure — a condition in which the heart can't circulate enough blood to meet the body's needs. These complications generally are reversible with appropriate treatment.
- Bones becoming brittle and prone to fractures. Untreated hyperthyroidism can also lead to weak, brittle bones (osteoporosis). The strength of the bones depends, in part, on the amount of calcium and other minerals they contain. Too much thyroid hormone interferes with the body's ability to incorporate calcium into the bones.
- Problems with eyes and vision. People with Graves' ophthalmopathy develop eye problems, including bulging, red or swollen eyes, sensitivity to light, and blurring or double vision. Untreated, severe eye problems can lead to vision loss.
- Red, swollen skin. In rare cases, people with Graves' disease develop Graves' dermopathy, which affects the skin, causing redness and swelling, often on the shins and feet.
- Thyrotoxic crisis. Hyperthyroidism also places one at risk of thyrotoxic crisis — a sudden intensification of the symptoms, leading to a fever, a rapid pulse and even delirium. If this occurs, seek immediate medical care
Goal of treatment is to reduce the level of thyroxine to normal. Other problems, such as a large goitre (thyroid swelling) or associated eye problems, may also need treatment. Factors such as the underlying cause of the problem, the age and the size of any goitre are taken into account to decide on the best treatment plan.
Options for treatment are:
Medicines
Drugs reduce the amount of thyroxine made by the overactive thyroid gland. The most common medicine used is carbimazole. Carbimazole does not affect the thyroxine which is already made and stored but reduces further production. Therefore, it may take 4 to 8 weeks of treatment for the thyroxine level to come down to normal. The dose of carbimazole needed to keep the thyroxine level normal varies from person to person. A high dose is usually given initially which is then reduced as the thyroxine levels come down.
It usually takes 12-18 months for the disease to settle down. After this, in about half of cases, the condition will have settled down and the carbimazole can be stopped. If the condition flares up again sometime in the future, a further course may be needed. However, in these cases an alternative treatment (for example, radioactive iodine) is often recommended. In about half of cases, carbimazole needs to be continued long-term to control symptoms. A different treatment may then be a better option if one does not want to take carbimazole long-term.
Radioiodine
In this procedure, a drink is given to patient, or he is asked to swallow a capsule, which contains radioactive iodine. The main use of iodine in the body is to make thyroxine. Therefore, the radioactive iodine builds up in the thyroid gland. As the radioactivity is concentrated in the thyroid gland, it destroys some thyroid tissue which reduces the amount of thyroxine that one make. The dose of radioactivity to the rest of the body is very low and is not dangerous. However, it is not suitable if one are pregnant or breast-feeding. In addition, after treatment, women should not become pregnant for at least six months and men are advised not to father children for at least four months.
Surgery
In this, a part of the thyroid gland is removed surgically. It may be a good option if one have a large thyroid swelling (goitre) which is causing problems in the neck. If too much thyroid tissue is removed then one will be given thyroxine tablets to keep the thyroxine level normal. It is usually a safe operation. But, as with all operations, there is a small risk.
Beta-blocker medicines
These type of medications are prescribed in some people for a few weeks whilst the level of thyroxine is reduced gradually by one of the above treatments. Symptoms of tremor, palpitations, sweating, agitation and anxiety reduce with beta blocker medications
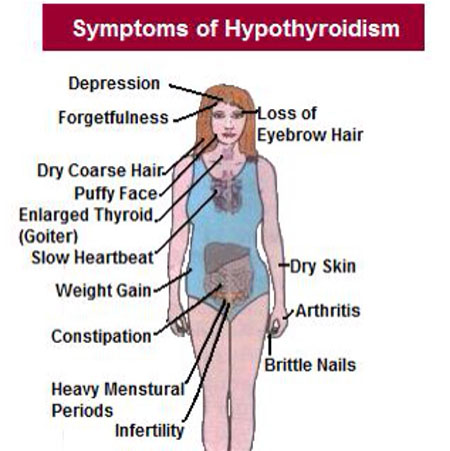
Hypothyroidism
Underactive thyroid gland is called as hypothyroidism. It is a term used to describe a condition in which there is a reduced level of thyroid hormone (thyroxine) in the body.
When thyroid gland is unable to make enough thyroxine it results in hypothyroidism. Hypothyroidism causes many of the body's functions to slow down.
When the thyroid gland fails to produce enough hormones it results in hypothyroidism. Hypothyroidism may be due to a number of factors, including:
- Autoimmune disease. People who develop a particular inflammatory disorder known as Hashimoto's thyroiditis suffer from the most common cause of hypothyroidism. Autoimmune disorders occur when the immune system produces antibodies that attack the own tissues. Sometimes this process involves the thyroid gland. Scientists aren't sure why the body produces antibodies against itself. Some think a virus or bacterium might trigger the response, while others believe a genetic flaw may be involved. Most likely, autoimmune diseases result from more than one factor. But however it happens, these antibodies affect the thyroid's ability to produce hormones.
- Hyperthyroidism treatment. People who produce too much thyroid hormone (hyperthyroidism) are often treated with radioactive iodine or anti-thyroid medications to reduce and normalize their thyroid function. However, in some cases, treatment of hyperthyroidism can result in permanent hypothyroidism.
- Surgery of thyroid gland. Removing all or a large portion of the thyroid gland can diminish or halt hormone production. In that case, you'll need to take thyroid hormone for life.
- Radiotherapy. Radiation used to treat cancers of the head and neck can affect the thyroid gland and may lead to hypothyroidism.
- Use of certain medications. A number of medications can contribute to hypothyroidism. One such medication is lithium, which is used to treat certain psychiatric disorders. If you're taking medication, ask the doctor about its effect on the thyroid gland.
Rarely, hypothyroidism may result from one of the following:
- Diseases arising due to birth defects. Some babies are born with a defective thyroid gland or no thyroid gland. In most cases, the thyroid gland didn't develop normally for unknown reasons, but some children have an inherited form of the disorder. Often, infants with congenital hypothyroidism appear normal at birth. That's one reason why most states now require newborn thyroid screening.
- Disorders of pituitary. A relatively rare cause of hypothyroidism is the failure of the pituitary gland to produce enough thyroid-stimulating hormone (TSH) — usually because of a benign tumor of the pituitary gland.
Risk factors
One is at increased risk to develop hypothyroidism if one or more of following risk factors are present:
- Woman older than age 60
- Autoimmune disease
- Family history of an autoimmune disease
- Treatment with radioactive iodine or anti-thyroid medications
- Having received radiation to the neck or upper chest
- Thyroid surgery
You may barely notice the symptoms of hypothyroidism at first, such as fatigue and weight gain, or you may simply attribute them to getting older. But as the metabolism continues to slow, you may develop more obvious signs and symptoms. Hypothyroidism signs and symptom may include:
- Puffy face
- Fatigue
- Increased sensitivity to cold
- Constipation
- Dry skin
- Hoarseness
- Muscle weakness
- Elevated blood cholesterol level
- Muscle aches, tenderness and stiffness
- Pain, stiffness or swelling in your joints
- Heavier than normal or irregular menstrual periods
- Thinning hair
- Slowed heart rate
- Depression
- Impaired memory
In untreated hypothyroidism, signs and symptoms can gradually become more severe. Myxedema is an advanced type of hypothyroidism. It is rare, but when it occurs it can be life-threatening. Signs and symptoms include low blood pressure, decreased breathing, decreased body temperature, unresponsiveness and even coma. In extreme cases, myxedema can be fatal.
Hypothyroidism can be diagnosed by a blood test. A normal blood test will also rule it out if symptoms suggest that it may be a possible diagnosis. One or both of the following may be measured:
- TSH. This hormone is made in the pituitary gland. It is released into the bloodstream. It stimulates the thyroid gland to make thyroxine. If the level of thyroxine in the blood is low, then the pituitary releases more TSH to try to stimulate the thyroid gland to make more thyroxine. Therefore, a raised level of TSH means the thyroid gland is underactive and is not making enough thyroxine.
- Thyroxine (T4). A low level of T4 confirms hypothyroidism.
In some people. TSH level is raised but they have a normal T4 level. This means that you are making enough thyroxine but the thyroid gland is needing extra stimulation from TSH to make the required amount of thyroxine. In this situation you have an increased risk of developing hypothyroidism in the future. The doctor may advise a repeat blood test every so often to see if you do eventually develop hypothyroidism. Other tests are not usually necessary unless a rare cause of hypothyroidism is suspected. For example, tests of the pituitary gland may be done if both the TSH and T4 levels are low.
Untreated hypothyroidism can lead to:
- An increased risk of developing heart disease. This is because a low thyroxine level causes the blood lipids (cholesterol, etc) to rise.
- An increased risk of developing some pregnancy complications - for example: pre-eclampsia, anaemia, premature labour, low birth weight, stillbirth, and serious bleeding after the birth.
- Chances of developing hypothyroid coma (myxoedema coma) which is a very rare complication.
With treatment, however, the outlook is excellent. With treatment, symptoms usually go, and you are very unlikely to develop any complications.
Hypothyroidism treatment involves daily use of the synthetic thyroid hormone levothyroxine. This oral medication restores adequate hormone levels, reversing the signs and symptoms of hypothyroidism.Treatment with levothyroxine is usually lifelong, but because the dosage you need may change, the doctor is likely to check the TSH level every year.
Determining proper dosage may take time. To determine the right dosage of levothyroxine initially, the doctor generally checks the level of TSH after two to three months.
Some drugs, supplements and even some foods may affect the ability to absorb levothyroxine. Talk to the doctor if you eat large amounts of soy products or a high-fiber diet or you take other medications, such as:
- Iron supplements
- Cholestyramine
- Aluminum hydroxide, which is found in some antacids
- Calcium supplements



