Disease Information
Stroke
Stroke happens when the blood supply to part of the brain is cut of. Without blood, brain cells can be damaged or die. This damage can have direct efects depending on where it happens in the brain. It can affect a person’s body, mobility and speech, as well as how they think and feel. About stroke worldwide
- Each year nearly 800,000 people experience a new or recurrent stroke.
- A stroke happens every 40 seconds.
- Stroke is the fifth leading cause of death in the U.S.
- Every 4 minutes someone dies from stroke.
- Up to 80 percent of strokes can be prevented.
- Stroke is the leading cause of adult disability in the U.S.
Stroke is a leading cause of death and disability globally. Stroke can happen to anyone at any age. It affects everyone: survivors, family and friends, workplaces and communities – but strokes are preventable. We all have a reason to prevent stroke – what's yours?

A stroke is a "brain attack". It occurs when blood flow to an area of brain is cut off. When this happens, brain cells are deprived of oxygen and begin to die. When brain cells die during a stroke, abilities controlled by that area of the brain such as memory and muscle control are lost. How a person is affected by their stroke depends on where the stroke occurs in the brain and how much the brain is damaged. For example, someone who had a small stroke may only have minor problems such as temporary weakness of an arm or leg. People who have larger strokes may be permanently paralyzed on one side of their body or lose their ability to speak. Some people recover completely from strokes, but more than 2/3 of survivors will have some type of disability.
Ischemic stroke
Ischemic stroke occurs when a blood vessel carrying blood to the brain is blocked by a blood clot. This causes blood not to reach the brain. High blood pressure is the most important risk factor for this type of stroke. Ischemic strokes account for about 87% of all strokes. An ischemic stroke can occur in two ways.
Embolic stroke
In an embolic stroke, a blood clot or plaque fragment forms somewhere in the body (usually the heart) and travels to the brain. Once in the brain, the clot travels to a blood vessel small enough to block its passage. The clot lodges there, blocking the blood vessel and causing a stroke. About 15% of embolic strokes occur in people with atrial fibrillation (Afib). The medical word for this type of blood clot is embolus.
Thrombotic stroke
A thrombotic stroke is caused by a blood clot that forms inside one of the arteries supplying blood to the brain. This type of stroke is usually seen in people with high cholesterol levels and atherosclerosis. The medical word for a clot that forms on a blood-vessel deposit is thrombus.
Two types of blood clots can cause thrombotic stroke: large vessel thrombosis and small vessel disease.
Hemorrhagic stroke
There are two types of stroke, hemorrhagic and ischemic. Hemorrhagic strokes are less common, in fact only 15 percent of all strokes are hemorrhagic, but they are responsible for about 40 percent of all stroke deaths. A hemorrhagic stroke is either a brain aneurysm burst or a weakened blood vessel leak. Blood spills into or around the brain and creates swelling and pressure, damaging cells and tissue in the brain. There are two types of hemorrhagic stroke called intracerebal and subarachnoid.
Inracerebral hemorrhage
The most common hemorrhagic stroke happens when a blood vessel inside the brain bursts and leaks blood into surrounding brain tissue (intracerebal hemorrhage). The bleeding causes brain cells to die and the affected part of the brain stops working correctly. High blood pressure and aging blood vessels are the most common causes of this type of stroke. Sometimes intracerebral hemorrhagic stroke can be caused by an arteriovenous malformation (AVM). AVM is a genetic condition of abnormal connection between arteries and veins and most often occurs in the brain or spine. If AVM occurs in the brain, vessels can break and bleed into the brain. The cause of AVM is unclear but once diagnosed it can be treated successfully
Subarachnoid hemorrhage
This type of stroke involves bleeding in the area between the brain and the tissue covering the brain, known as the subarachnoid space. This type of stroke is most often caused by a burst aneurysm. Other causes include:
- • Bleeding disorders
- • Head injury
- • Blood thinners
When blood flow to part of the brain stops for a short period of time, also called transient ischemic attack (TIA), it can mimic stroke-like symptoms. These symptoms appear and last less than 24 hours before disappearing. While TIAs generally do not cause permanent brain damage, they are a serious warning sign that a stroke may happen in the future and should not be ignored.
TIA are usually caused by one of three things:
- 1. Low blood flow at a narrow part of a major artery carrying blood to the brain.
- 2. A blood clot in another part of the body (such as the heart) breaks off, travels to the brain, and blocks a blood vessel in the brain.
- 3. Narrowing of the smaller blood vessel in the brain, blocking blood flow for a short period of time; usually caused by plaque (a fatty substance) build-up.
Some important facts to keep in mind include:
- 40 percent of people who have a TIA will have an actual stroke
- Nearly half of all strokes occur within the first few days after a TIA
- Symptoms for TIA are the same as for a stroke
- The goal of TIA management is to prevent a future stroke. The medicine and therapy used depends on the exact cause of the TIA. In addition to lifestyle changes such as diet, physical activity, limiting alcohol intake, and not smoking, your healthcare provider may recommend medications to treat high blood pressure, high cholesterol, or heart disease. These changes may reduce your risk of further TIA or stroke.
There are many medications that help prevent blood clots from forming—reducing the risk of full-blown stroke.
If a TIA is caused by blockage in the main artery in the neck that supplies blood to the brain, called the carotid artery, surgeries may be required to open the artery, and prevent a stroke. These procedures are known as endarterectomy and stenting.
Talk to a healthcare provider about the best stroke prevention options for you. The lifestyle adjustments such as eating healthy foods and quitting smoking—made today may reduce the risk of stroke tomorrow
What is the FAST test for a stroke?If You're at Risk for a Stroke, This Acronym Could Save Your Life
FAST is an acronym used for all of us to remember what to look for if we think someone is having a stroke. The “F” stands for face. That means when asking a person to smile, you should pay attention to any asymmetry in their face. The “A” stands for arms. So, ask them to hold up both of their arms and see if one side drifts down or is not quite as high as the other side. The “S” stands for speech. Post-stroke speech is either slurring of words or difficulty coming up with the appropriate word or even understanding. The “T” stands for time, as in, if you notice any of the first three things, it's time for urgent medical help .Time is very critical because every minute a person has a blockage in the blood vessel, they’re losing 1.9 million brain cells.
Other warning signs
- sudden trouble seeing in one or both eyes
- sudden numbness or weakness of your face, arm, and leg, most likely on one side of your body
- sudden confusion or unconsciousness
- sudden and severe headache with no known cause
- sudden dizziness, trouble walking, or loss of balance or coordination
A silent stroke is a stroke with no or mild symptoms , they are often discovered incidentally. For example, you might have a severe headache, and the doctor will take some images of your brain using a CT scan or MRI. If you’ve had a silent stroke, these images may show evidence of a brain insult or scar tissue. The doctor will probably ask you if you’ve had any stroke symptoms such as weakness, numbness, tingling, inability to speak, inability to see and if the symptoms were transient, but you may not remember having any of the symptoms.
Headaches can be unrelated to stroke, but a sudden, severe headache with loss of vision or numbness in the face may be a sign of a stroke .Headaches are more consistent with bleeding strokes (hemorrhage strokes). If somebody comes into the hospital with a sudden headache and weakness, I would expect this to be the bleeding kind of stroke. If there is no headache, I will probably lean towards the ischemic stroke, which is associated with blood clots.Is there a risk of stroke during a migraine attack? Understandably, some people are afraid that their migraine is a symptom of a stroke and others worry that they are more at risk of a stroke during a migraine attack. There is little evidence to suggest that a stroke is more likely to occur during a migraine attack than at another time. Migraine is common. In some people migraine and stroke appear together but the nature of the causal relationship, if any, is difficult to establish firmly. Migrainous infarction is the term given to an ischaemic stroke occurring during a migraine attack.
However, research suggests that such a stroke would be independent of the migraine attack. It is also possible for a person to have a stroke but for this to have been mistaken for a migraine attack. The migraine aura can mimic transient ischaemic attacks (TIAs). Conversely, in stroke, headache similar to migraine may occur.
Would I worry about every headache being a stroke? No, but there is about is about a 20-30% chance that having a stroke will lead to a headache.
Stroke is on the rise among younger adults – 15% of ischemic strokes occur in young adults and adolescents.The financial burden and family obligations after a stroke in young adults can be significantly more than for older stroke survivors. Young adults often can’t identify stroke symptoms or they ignore them, resulting in more severe outcomes or loss of life. The financial burden and family obligations after a stroke in young adults can be significantly greater than for older stroke survivors. Because of their younger age, they will frequently live longer with the physical effects of a stroke and experience a greater loss in salary earnings over a longer period of time. There was a 44% increase in the number of young patients hospitalized due to stroke over the last decade. It’s important to get involved, take action to prevent strokes or share your story to give other young stroke survivors hope and encouragement.
Here are some of the common myths about strokes:
Myth: Strokes are not preventable.
Fact: Up to 80% of strokes can be prevented
Myth:Strokes cannot be treated.
Fact: There are a number of stroke treatments, but immediate treatment is the key to success.
Myth: Strokes happen only in the elderly.
Fact: Anyone can have a stroke. , About 12 % of stroke occurs in young
Myth: Strokes happen in the heart.
Fact: Strokes happen within the brain, when the blood supply is cut off.
Myth: If you haven't recovered from a stroke in six months, you won't recover any further.
Fact: : Stroke recovery can continue a whole lifetime.
Myth: If stroke symptoms go away, you don’t have to see a doctor.
Fact: Temporary stroke symptoms are called transient ischemic attacks (TIA). They are warning signs prior to actual stroke and need to be taken seriously
Immediate treatment for a stroke is critical because brain cells die when they no longer receive oxygen and nutrients from the blood; They also are damaged by sudden bleeding into or around the brain. When blood flow to the brain is interrupted, some brain cells die immediately, while others remain at risk for dying.If you experience the sudden onset of neurological symptoms, Do not waste precious time , by unnecessary delaying in treatment. Earlier you receive treatment better is the chances of recovery .
Uncontrolled hypertension (high blood pressure) causes the rupture of blood vessels in the brain, leading to a stroke involving bleeding in the brain. Uncontrolled hypertension can contribute to decreased blood flow in the small blood vessels located deep inside the brain, as well as stroke.
People with diabetes, high blood pressure, high cholesterol, are at a higher risk for stroke .Other illnesses like irregular heartbeat can increase your chances of stroke. There are many other risk factors for stroke, including obesity, snoring ( Obstructive sleep Apnea ) etc .
Over time, high blood pressure and diabetes can weaken the blood vessels, causing them to burst. High cholesterol can lead to fat buildup in the arteries, which can decrease blood flow. People who have already had a stroke are also more likely to suffer another one.
Did you know that 90% of strokes are linked to 10 avoidable risks ? If you have diabetes, heart problems or history of stroke/TIA talk to your doctor about stroke risk and preventive treatments.
- 1. Control high blood pressure
- 2. Do moderate exercise 5 times a week
- 3. Eat a healthy, balanced diet (high in fruit/vegetables, low in sodium)
- 4. Reduce your cholesterol
- 5. Maintain a healthy BMI or waist to hip ratio
- 6. Stop smoking and avoid second-hand exposure
- 7. Reduce alcohol intake
- 8. Identify and treat atrial fibrillation (heart beat irregularity )
- 9. Reduce your risk from diabetes, talk to your doctor
- 10. Get educated about stroke
Walking not only improves the quality of life for someone who has suffered from a stroke, but also builds endurance .
Stroke affects everyone – we all have a reason to prevent it
Stroke is the third leading cause of death for women (in comparison, stroke is the fifth leading cause of death for men). Each year 55,000 more women have a stroke than men. Because in general women live longer than men, stroke will have a more negative impact on their lives. More women will
- Live alone when they have a stroke
- Be more likely to live in a long term health care facility after a stroke
- Have a worse recovery after stroke
Apart from common symptoms unique symptoms in women are:
- Loss of consciousness or fainting
- General weakness
- Difficulty or shortness of breath
- Confusion, unresponsiveness or disorientation
- Sudden behavioral change
- Agitation
- Hallucination
- Nausea or vomiting
- Pain
- Seizures
- Hiccups
Unique risk factors in women are -.In addition to the general risk factors like family history, high blood pressure, high cholesterol, diabetes, smoking, lack of exercise, and being overweight, as a woman you are faced with unique risk factors which include:
- Taking birth control pills. The greatest concern about using oral contraceptives is for women with additional risk factors, such as age, cigarette smoking, high blood pressure or diabetes.
- Being pregnant. Stroke risk increases during a normal pregnancy due to natural changes in the body such as increased blood pressure and stress on the heart.
- Using Hormone Replacement Therapy (HRT), a combined hormone therapy of progestin and estrogen, to relieve menopausal symptoms.
- Suffering from migraine headaches with aura. Migraines can increase a woman's stroke risk two and a half times and most people in the U.S. who suffer migraines are women.
Sroke prevention in women
Each year stroke kills twice as many women as breast cancer. However, this fact is widely unknown among the general public. Women are also less knowledgeable about the risk factors and don’t perceive themselves at risk for stroke.
- Women who experience migraines with aura and smoke are advised to stop smoking immediately.
- Women who are pregnant should monitor their blood pressure during and after pregnancy to lower the risk of stroke.
- Women over 75 should be screened for Atrial Fibrillation
- Women should be screened for high blood pressure prior to starting a birth control regimen.
- Women with concerns about high blood pressure or stroke should consult a doctor.
Alzheimer's and Dementia
In India, more than 4 million people have some form of dementia & Worldwide, at least 44 million people are living with dementia, making the disease a global health problem that must be addressed.A diagnosis of Alzheimer’s is life changing for the person with the disease, as well as their family and friends .
Alzheimer's disease is the most common type of dementia. Alzheimer’s causes problems with memory, thinking and behavior. In the early stage, dementia symptoms may be minimal, but as the disease causes more damage to the brain, symptoms worsen. The rate at which the disease progresses is different for everyone.
There are currently no treatments to stop Alzheimer’s disease from progressing, there are medications to treat dementia symptoms. In the past three decades, dementia research has provided a much deeper understanding of how Alzheimer’s affects the brain. Today, researchers are continuing to look for more effective treatments and a cure, as well as ways to prevent Alzheimer’s and improve brain health.
Trouble with memory—specifically difficulty recalling information that has recently been learned—is often the first symptom of Alzheimer’s disease.
As we grow older, our brains change, and we may have occasional problems remembering certain details. However, Alzheimer’s disease and other dementias cause memory loss and other symptoms serious enough to interfere withday-to-day life activities.
Not all memory loss is caused by Alzheimer’s.
If you or someone you know is experiencing problems with memory or other symptoms of dementia, see a doctor. Some causes of symptoms, such as medication side effects and vitamin deficiencies, are reversible.
In addition to memory loss, symptoms of Alzheimer’s include:
- Trouble completing tasks that were once easy.
- Difficulty solving problems.
- Changes in mood or personality; withdrawing from friends and family.
- Problems with communication, either written or spoken.
- Confusion about places, people and events.
- Visual changes, such trouble understanding images.
Family and friends may notice the symptoms of Alzheimer’s and other progressive dementias before the person himself experiencing these changes. If you or someone you know is experiencing possible symptoms of dementia, it is important to seek a medical evaluation to find the cause.
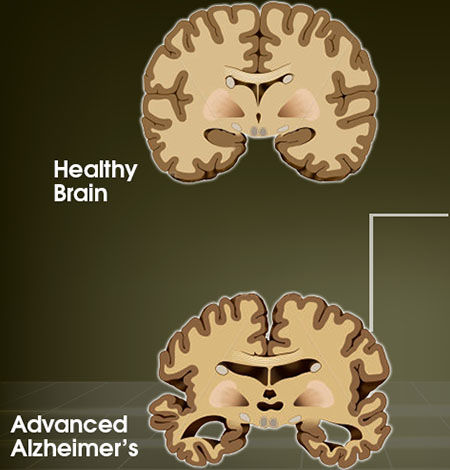
Alzheimer’s and the changes in Brain
Brain cells in the hippocampus, a part of the brain associated with learning, are often the first to be damaged by Alzheimer’sdisease . This is why memory loss, especially difficulty remembering recently learned information, is often the first symptom of the disease.
We do not understand all the reasons some people develop Alzheimer’s disease while others do not, research has given us a better understanding of which factors put someone at a higher risk.
- Age. Advancing age is the greatest risk factor for developing Alzheimer’s disease. The majority of people diagnosed with Alzheimer's disease are 65 or older. Although far less common, younger-onset Alzheimer’s (also known as early-onset Alzheimer’s) affects people younger than 65. It is estimated that up to 5 percent of people with Alzheimer’s have younger-onset disease. Younger-onset Alzheimer’s is often misdiagnosed.
- Family Members with Alzheimer’s. If your parent or sibling develops Alzheimer’s, you are more likely to develop the disease than someone who does not have a first-degree relative with Alzheimer’s. Scientists do not completely understand what causes Alzheimer’s to run in families, but genetics, environmental factors and lifestyle may all play a part.
- Genetics.Researchers have identified several gene variants that increase the chance of developing Alzheimer’s disease. The APOE-e4 gene is the most common risk gene associated with Alzheimer’s; it is estimated to play a role in as many as one-quarter of Alzheimer’s cases.
Deterministic genes are different than risk genes in that they guarantee someone will develop a disease.
The only known cause of Alzheimer’s is from inheriting a deterministic gene. Alzheimer’s caused by a deterministic gene is rare, and likely occurs in less than 1 percent of Alzheimer’s cases. When a deterministic gene causes Alzheimer’s, it is called “autosomal dominant Alzheimer’s disease (ADAD).” - Mild Cognitive Impairment (MCI). The symptoms of MCI include changes in the ability to think, but these symptoms do not interfere with everyday life and are not as severe as those caused by Alzheimer’s or other progressive dementias. Having MCI, particularly MCI that involves memory problems, increases the risk of developing Alzheimer’s and other dementias. However, MCI does not always progress. In some cases, it reverses or remains stable.
- Cardiovascular Disease. Research suggests that brain health is closely related to heart and blood vessel health. The brain gets the oxygen and nutrients needed to function normally from blood, and the heart is responsible for pumping blood to the brain. Therefore, factors that cause cardiovascular disease also may be linked to a higher risk of developing Alzheimer’s and other dementias, including smoking, obesity, diabetes, and high cholesterol and high blood pressure in midlife.
- Education and Alzheimer’s. Studies have linked fewer years of formal education with an increased risk of Alzheimer’s and other dementias. There is not a clear reason for this association, but some scientists believe more years of formal education may help increase connections between neurons, allowing the brain to use alternative routes of neuron-to-neuron communication when changes related to Alzheimer’s and other dementias occur.
- Traumatic Brain Injury. The risk of Alzheimer’s disease and other dementias increases after a moderate or severe traumatic brain injury, such as a blow to the head or injury of the skull that causes amnesia or loss of consciousness for more than 30 minutes. Fifty percent of traumatic brain injuries are caused by motor vehicle accidents. Individuals who sustain repeated brain injuries, such as athletes and those in combat, are also at a higher risk of developing dementia and impairment of thinking skills.
Is there an Alzheimer’s test?
There is no simple way to detect Alzheimer’s. Diagnosis requires a complete medical exam. Blood tests, mental status tests and brain imaging may be used to determine the cause of symptoms.
- Your family’s medical history
- A neurological exam
- Cognitive tests to evaluate memory and thinking
- Blood tests (to rule out other possible causes of symptoms)
- Brain imaging
While doctors can usually determine if someone has dementia, it may be more difficult to distinguish what type of dementia. Misdiagnosis is more common with younger-onset Alzheimer’s.
Receiving an accurate diagnosis earlier in the disease process is important because it allows:
- A higher likelihood of benefiting from available treatments, which can improve quality of life
- The opportunity to receive support services
- A chance to participate in clinical trials and studies
- An opportunity to express wishes regarding future care and living arrangements
- Time to put financial and legal plans in place
While there are currently no treatments available to slow or stop the brain damage caused by Alzheimer’s disease, several medications can temporarily help improve the symptoms of dementia for some people. These medications work by increasing neurotransmitters in the brain.
Researchers continue to search for ways to better treat Alzheimer’s and other progressive dementias. Currently, dozens of therapies and pharmacologic treatments that focus on stopping the brain cell death associated with Alzheimer’s are underway.
In addition, having support systems in place and the use of non-pharmacologic behavioral interventions can improve quality of life for both people with dementia and their caregivers and families. This includes:
- • Treatment of co-existing medical conditions
- • Coordination of care among health care professionals
- • Participation in activities, which can improve mood
- • Behavioral interventions (to help with common changes, such as aggression, sleep issues and agitation)
- • Education about the disease
- • Building a care team for support
Providing care for someone with Alzheimer’s disease or another dementia can be both rewarding and challenging. In the early stages of dementia, a person may remain independent and need very little care. However, as the disease progresses, care needs will intensify, eventually leading to a need for around-the-clock assistance.
We often hear from caregivers and family members that one of the most upsetting aspects of Alzheimer’s is the changes in behavior it causes. Many resources are available to help caregivers know what to expect and how to adapt during the early, middle and late stages of the disease.
Epilepsy
Epilepsy also known as seizure disorder, is a disorder of the brain. A person is diagnosed with epilepsy when they have had two or more seizures

A seizure is caused by disturbances in electrical activity of the brain . Some seizures can look like staring spells. Other seizures cause a person to fall, shake, and lose awareness of what’s going on around them. Many different things can occur during a seizure. Whatever the brain and body can do normally can also occur during a seizure
What happens during a seizure ?
- Seizures can take on many different forms, and seizures affect different people in different ways.
- Not all parts of a seizure may be visible or easy to separate from each other. Every person with seizures will not have every stage or symptom.
- An aura or warning is the first symptom of a seizure and is considered part of the seizure. Not everyone has an aura.
- The middle of a seizure is often called the ictal phase. This correlates with the electrical seizure activity in the brain.
- As the seizure ends, the postictal phase occurs - this is the recovery period after the seizure. Some people recover immediately while others may take minutes to hours to feel like their usual self.
A risk factor is something that makes a person more likely to develop seizures and epilepsy. Sometimes a risk factor can cause scarring of the brain or lead to areas of the brain not developing or working right
- Babies who are born small for their age
- Babies who have seizures in the first month of life
- Babies who are born with abnormal areas in the brain
- Bleeding into the brain
- Abnormal blood vessels in the brain
- Serious brain injury or lack of oxygen to the brain
- Brain tumors
- Infections of the brain: abscess, meningitis, or encephalitis
- Stroke resulting from blockage of arteries
- Cerebral palsy
- Conditions with intellectual and developmental disabilities
- Seizures occurring within days after head injury ("early posttraumatic seizures")
- Family history of epilepsy or fever-related seizures
- Alzheimer's disease (late in the illness)
- Autism spectrum disorder
- Fever-related (febrile) seizures that are unusually long
- Long episodes of seizures or repeated seizures called status epilepticus
- Use of illegal drugs such as cocaine
- Head injuries, such as a concussion with just a very brief loss of consciousness, do not cause epilepsy.
What if I don’t have any of those risk factors?
Although the disorders and injuries on these lists help to explain many cases of epilepsy, more people with epilepsy don't have any of these. Often we just don't know how or why epilepsy gets started.
Even though you may not know the cause of your epilepsy, you can look at whether there are factors (often called "triggers") that precipitate or provoke seizures. These triggers may make a person with epilepsy more likely to have a seizure in certain situations. The triggers could change the number or severity of seizures. Learning if you have any triggers can help you learn what to do next. Sometimes people can learn how to modify their lifestyle or environment to lessen the risk of triggers.
- Missed medication
- Lack of sleep or disrupted sleep
- Illness (both with and without fever)
- Psychological stress
- Heavy alcohol use or seizures after alcohol withdrawal
- Use of cocaine and other recreational drugs such as Ecstasy
- Over-the-counter drugs, prescription medications or supplements that decrease the effectiveness of seizure medicines
- Nutritional deficiencies: vitamins and minerals
- Poor eating habits, such as long times without eating, dehydration or not enough fluids
- The menstrual cycle or hormonal changes
- Flashing lights or patterns
- Specific activities, noises or foods
How long do seizures usually last?
Usually, a seizure lasts from a few seconds to a few minutes. It depends on the type of seizure.
A person having a seizure may seem confused or look like they are staring at something that isn’t there. Other seizures can cause a person to fall, shake, and become unaware of what’s going on around them.
Seizures are classified into two groups.
- 1. Generalized seizures affect both sides of the brain.
- 2. Focal seizures affect just one area of the brain. These seizures are also called partial seizures.
A person with epilepsy can have more than one kind of seizure
Not always. Seizures can also happen because of other medical problems. These problems include.
- High fever.
- Low blood sugar.
- Alcohol or drug withdrawal.
Epilepsy can be caused by different conditions that affect a person’s brain. Some known causes include
- Stroke.
- Brain tumor.
- Brain infection, like Neurocysticercosis
- Traumatic head injury.
- Loss of oxygen to the brain (for example, during birth).
- Some genetic disorders (such as Downs Syndrome).
- Other neurologic diseases (such as Alzheimers ).
For 2 in 3 people, the cause of epilepsy is unknown. This type of epilepsy is called cryptogenic or idiopathic.
Is epilepsy common?
Epilepsy is one of the most common neurologic disorders, affecting up to 1% of the population.
Many tests are commonly done to diagnose epilepsy or seizure disorder . For example , to understand the underlying electrical abnormality of the brain EEG is done routinely . Again , there are different types of EEG . Whenever there is doubt – that the seizure is genuine electrical abnormality or pseudoseizure , Video EEG often helps in such situation . Another type of EEG called Long term EEG is often done to get the maximum abnormalities possible from the graph . Many a time Video EEG & Long term EEG is done to Classify the type & pattern of seizure which helps in planning & execution of treatment . Other than several blood tests , investigation like MRI brain is often required to know about the structural abnormalities of brain .
How can I prevent epilepsy?
Yes , epilepsy can be prevented .
- Have a healthy pregnancy. Some problems during pregnancy and childbirth may lead to epilepsy. Follow a prenatal care plan with your health care provider to keep you and your baby healthy.
- Prevent brain injuries
- Lower the chances of stroke & heart disease
- Be up-to-date on your vaccinations
- Wash your hands and prepare food safely to prevent infections such as cysticercosis.
How is epilepsy diagnosed?
A person who has a seizure for the first time should talk to a health care provider, such as a doctor or nurse practitioner. The provider will talk to the person and will refer him or her to a Neurologist who will diagnose & plan for treatment .
How is epilepsy treated?
The most common treatments for epilepsy are
- Medicine. Anti-seizure drugs are medicines that limit the spread of seizures in the brain. A Neurologist will prescribe a drug if needed. Surgery. When seizures not easily controlled by medicines, and come from a single area of the brain (focal seizures), surgery to remove that area may stop future seizures or make them easier to control with medicine. Epilepsy surgery is mostly used when the seizure focus is located in the temporal lobe of the brain.
- Other treatments. When medicines do not work and surgery is not possible, other treatments can help. These include vagus nerve stimulation, where an electrical device is placed, or implanted, under the skin on the upper chest to send signals to a large nerve in the neck. Another option is the ketogenic diet, a high fat, low carbohydrate diet with limited calories.
Who treats epilepsy?
Primary care providers such as family physicians, pediatricians, and nurse practitioners are often the first people to see a person with epilepsy . These providers may make the diagnosis of epilepsy or they may refer to a neurologist
A neurologist is a doctor who specializes in the brain and nervous system .People who have seizures that are difficult to control or who need advanced care for epilepsy may be referred to an epilepsy centers. Epilepsy centers are staffed by providers who specialize in epilepsy care, such as
- Epileptologists and neurologists.
- Nurses.
- Psychologists.
- Technicians.
What can I do to manage my epilepsy?
Begin with these tips:
- Take your medicine regularly
- Talk with your doctor or nurse when you have questions.
- Recognize seizure triggers (such as flashing or bright lights).
- Keep a record of your seizures.
- Get enough sleep.
- Lower stress.
Epilepsy is a form of spiritual possession.
Although most people have recognized that epilepsy is not a form of possession, some cultures still believe this. Epilepsy organizations are working hard to educate all people that epilepsy is a medical condition.
You can swallow your tongue during a seizure.
It is physically impossible to swallow your tongue.
- You should force something into the mouth of someone having a seizure. Absolutely not! While doing that you may break your teeth, puncture gums,or even break someone’s jaw. The first aid is ,gently roll the person on one side and put something soft under his or head for protection from injury.
- You should restrain someone having a seizure. You should never use restraint! The seizure will run its course, and you cannot stop it.
- Epilepsy is contagious. It is false. Itcannot be ‘caught’ by coming into contact with someone who has seizures .
- Only kids get epilepsy. Epilepsy happens to people over age 65 almost as often as it does to children age 10 and under. Seizures in the elderly are often the after effect of other health issues like stroke and heart disease.
- People with epilepsy are disabled and can’t work. People with epilepsy have the same range of abilities and intelligence as the rest of us. Some have severe seizures and cannot work; others are successful and productive in challenging careers.
- People with epilepsy shouldn’t be in jobs of responsibility and stress. People with seizure disorders are found in all walks of life and at all levels in business, government, the arts and other professions. We aren’t aware of them because many people, even today, do not talk about having epilepsy for fear of what others might think.
If I have epilepsy, can I exercise and play sports?
Exercise is rarely a “trigger” for seizure activity. In fact regular exercise may improve seizure control. Safely playing sports can also be great for your physical, mental, and emotional well-being.
Are there special concerns for women who have epilepsy?
Women who have epilepsy face special challenges .For women with epilepsy, there are also special concerns about pregnancy, because having a seizure and taking certain drugs during pregnancy may increase the risk of harm to the baby. Women can take the following steps before and during pregnancy to lessen these risks. If you are a woman with epilepsy who plans to get pregnant, talk with your health team about how to best care for yourself and your baby.
Can a person die from epilepsy?
Most people with epilepsy live a full life. However, the risk of early death is higher for some. We know that the best possible seizure control and living safely can reduce the risk of epilepsy-related death.
Factors that can increase the risk of early death include
- More serious problems , such as a stroke or a tumor. These conditions carry an increased risk of death and may cause seizures.
- Falls or other injuries that happen because of seizures. These injuries can be life-threatening.
- Seizures that last over 5 minutes. This is a condition called status epilepticus. Status epilepticus can sometimes happen when a person suddenly stops taking seizure medication.
Rarely, people with epilepsy can experience sudden unexpected death in epilepsy (SUDEP). SUDEP is not well understood and experts don’t know what causes it, but they suspect that it is sometimes due to a change in heart beats (rhythm) during a seizure. Sudden death due to heart rhythm changes also happens in people who do not have seizures.
The risk of sudden death is larger for people with major uncontrolled seizures.
If I have epilepsy, can I exercise and play sports?
Exercise is rarely a “trigger” for seizure activity. In fact regular exercise may improve seizure control. Safely playing sports can also be great for your physical, mental, and emotional well-being
Migraine
Migraine is a neurological condition that can cause multiple symptoms. It’s frequently characterized by intense, debilitating headache . Symptoms may include nausea, vomiting, difficulty speaking, numbness or tingling, and sensitivity to light and sound. Migraine often run in families and affect all ages.
The diagnosis of migraine headache is determined based on clinical history, reported symptoms, and by ruling out other causes. The most common categories of migraine headache are those without aura (previously known as common migraines) and those with aura (previously known as classic migraines).
Migraines can begin in childhood or may not occur until early adulthood. Women are more likely than men to have migraine. Family history is one of the most common risk factors for having migraine.
How common is Migraine ?
According to A RESULT OF Survey in India 14 % of girls and 9 % of boys are affected by Migraine In 11 -15 year age Group.According to WHO Report IN Asia 3 % of Men and 10 % of women suffer from Migraine.
How many types of migraine are there ?
There are two types of migraine without aura and with aura. Migraine without aura is usually not associated with other neurological signs & symptoms. The headache is preceded by premonitory warning signs like changes in mood and energy levels. Headache takes sometimes to peak persisting for 4-24 hours if not intervened by medicine. However in Migraine patients with aura (Migraine associated with other neurological signs & Symptoms) see wavy or jagged lines, dots, tingling sensation in hand and leg and flashing lights in front of eyes.
Migraine symptoms may begin before the headache itself. This is known as the prodrome stage. Symptoms during this stage can include:
- food cravings
- depression
- fatigue or low energy
- frequent yawning
- hyperactivity
- irritability
- neck stiffness
In migraine with aura, the aura occurs after the prodrome stage. During an aura, you may have problems with your vision, sensation, movement, and speech. Examples of these problems include:
- difficulty speaking clearly
- feeling a prickling or tingling sensation in your face, arms, or legs
- seeing shapes, light flashes, or bright spots
- temporarily losing your vision
The next phase is known as the attack phase. This is the most acute or severe of the phases when the actual migraine pain occurs. In some people, this can overlap or occur during an aura. Attack phase symptoms can last anywhere from hours to days. Symptoms of migraine can vary from person to person. Some symptoms may include:
- increased sensitivity to light and sound
- nausea
- dizziness or feeling faint
- dizziness or feeling faint
- pain on one side of your head, either on the left side, right side, front, or back, or in your temples
- pulsing and throbbing head pain
- vomiting
After the attack phase, a person will often experience the postdrome phase. During this phase, there are usually changes in mood and feelings. These can range from feeling euphoric and extremely happy, to feeling very fatigued and apathetic. A mild, dull headache may persist.
People describe migraine pain as:
- pulsating
- throbbing
- perforating
- pounding
- debilitating
It can also feel like a severe dull, steady ache. The pain may start as mild, but without treatment it will become moderate to severe.
Migraine pain most commonly affects one side of the head, but it can occur on both sides, or shift.
Most migraine last about 4 hours. If they’re not treated or don’t respond to treatment, they can last for as long as 72 hours to a week. In migraine with aura, pain may overlap with an aura or may never occur at all.
Doctors diagnose migraines by listening to your symptoms, taking a thorough medical and family history, and performing a physical exam to rule out other potential causes. Imaging scans, such as a CT or MRI, can rule out other causes, including:
- tumours
- abnormal brain structures
- stroke
Yes, migraines have a tendency to run in families. Four out of five migraine sufferers have a family history of migraines.
- Many people find it difficult to identify triggers of migraine but potential triggers include bright lights, loud noise, certain odors or perfumes, weather & stress,
- Skipping meals, even some specific foods & beverages can also be associated as trigger in many people suffering from migraine. Identifying those Foods is essential to avoid migraine attack.
- Smoking, excessive intake of caffeine and Alcohol,
- Exposure to sunlight and extreme heat or cold
- Hormone fluctuations during menstrual period
- You need to find out what triggers affects you as potential triggers vary from person to person suffering from migraine.
- Keeping a headache diary is an effective way to track triggers as it helps you talk to your doctor about your condition.
Very often severity of a migraine attack makes people fear they are having a stroke. Migraine do not cause stroke but there is a rare association of migraine with brain stroke (brain attack).
Is migraine a life threatening condition? Is it curable ?
Migraine is a benign neurologicalcondition; not a life threatening condition.Yes, it can be easily controlled. Consult your doctor for further plan of treatment. He or she will be able to diagnose your particular type of Headache, decide whether further evaluation is needed and make recommendations about treatment.
Almost everyone has occasional headaches. Most headaches go away on their own. However;if you have Very frequent headaches that come in attacks, the headaches last anywhere from four to 24 hours, if they finds difficulty towards sensitivity of lights,noise,nausea, vomiting or loss of appetite associated with the onset of pain, you should consult a neurophysician.
Over The Counter or OTC medicine may be effective in reliving migraine pain for some people taken in the initial stage of experiencing symptom. You must consult a Neurophysician since medication and treatment plan for migraine varies from person to person, medicine reliving pain of one person may not be the same for other.
- Migraine is commonly misdiagnosed as sinus headache.
- Self-diagnosed sinus headache is nearly always migraine (90% of the time).
- Migraine is commonly associated with forehead and facial pressure over the sinuses, nasal congestion and runny nose. “True” sinus headache, more properly called rhinosinusitis, is relatively rare and secondary to a viral or bacterial sinus infection characterized by thick, discolored nasal discharge, possibly decreased smell or no smell, facial pain or pressure and commonly fever. Facial pain and headache should resolve within seven days after remission of viral symptoms or after successful treatment with antibiotics if a bacterial sinus infection is present. In the absence of fever, pus from your nose, alteration in smell or foul-smelling breath, you likely have a migraine headache. If pain continues,or becomes episodic then your diagnosis should be reconsidered.
- So, how do you know if your headache is migraine and not sinus? Ask yourself the following questions:
- In the last three months, how disabling are your headache ? Do they interfere with your ability to function? (Are you missing work; school; family activities?)
- Are your headaches ever associated with nausea?
- Are your headaches ever associated with sensitivity to light?
A vestibular migraine is a nervous system problem that causes repeated dizziness(or vertigo) in people who have a history of migraine symptoms. You may not always have a headache.
Ophthalmoplegic migraine headaches include pain around the eye along with paralysis of the muscles around it. In addition to headache, symptoms of ophthalmoplegic migraine include dilation of the pupils, inability to move the eye upward, downward or across, as well as a drooping of the upper eyelid
Periodic disorders of childhood often represent precursors of migraine. There is often a positive family history of migraine in children that present with periodic syndromes .They include
- Cyclical vomiting with migraine (periodic syndrome). This is characterised by recurrent episodes of intense vomiting occurring often at night and with complete recovery in between attacks. Girls are more affected. Stress and dietary triggers may be identified. It typically begins in toddlers.
- Abdominal migraine. This presents typically as recurrent bouts of generalised abdominal pain associated with nausea and vomiting but no headache, followed by sleep and recovery. Typical migraines may occur separately.
- Benign paroxysmal vertigo. This is seen usually from age 2-6 years and is characterised by brief episodes of vertigo and nausea with no hearing loss or loss of consciousness. More common migraine eventually ensues but referral to exclude posterior fossa tumours is required.
- Eat healthy fruits & Vegetables that contains vitamin B which helps in preventing migraine.
- Drink plenty of water to keep yourself hydrated & reduce intake of caffeine.
- Don’t Skip meals especially breakfast and eat frequent meals to avoid low blood sugar
- Have regular sleep. Disturbances in regular sleep pattern may trigger headache in many people
- Wear sunglasses/hat in bright sunlight .Good sunglasses is essential for eye health and lower migraine
- Rest your eyes occasionally while watching TV or using Computer.
- Some of the food, beverages can also be associated as trigger in many people suffering migraine. Identifying those Foods is essential to avoid migraine attack
Migraine can’t be cured, but your doctor can help you manage them, so you get them less often and treat symptoms when they occur. Treatment can also help to reduce the severity of headache .
Your treatment plan depends on:
- your age
- how often you have migraine
- the type of migraine you have
- how severe they are, based on how long they last, how much pain you have, and how often they prevent you from going to school or work.
- whether they include nausea or vomiting, as well as other symptoms
- other health conditions you may have and other medications you are on
Your treatment plan may include a combination of these:
- self-care
- lifestyle adjustments, including stress management and avoiding triggers .
- migraine medications, such as NSAIDs or acetaminophen or other combinations
- medications that you take every day to help prevent migraine and reduce how often you have headache
- medications that you take as soon as a headache starts, to keep it from becoming severe and to ease symptoms
- medications to help with nausea or vomiting
- hormone therapy if migraines seem to occur during mensturation cycle.
- counseling
- alternative care, which may include biofeedback , meditation, acupressure, or accupuncture
Obstructive sleep Apnea
Obstructive sleep apnea is a sleep disorder. It causes breathing to repeatedly stop and start during sleep.
There are several types of sleep apnea, but the most common is obstructive sleep apnea. This type of apnea occurs when your throat muscles intermittently relax and block your airway during sleep. A noticeable sign of obstructive sleep apnea is snoring.Treatments for obstructive sleep apneaare available. One treatment involves using a device that keep your airway open while you sleep. Another option is a mouthpiece to thrust your jaw forward during sleep. In more severe cases, surgery may be an option too.
Obstructive sleep apnea occurs when the muscles in the back of your throat relax too much to allow normal breathing. These muscles support structures including the soft palate, the uvula — a triangular piece of tissue hanging from the soft palate, the tonsils and the tongue.
When the muscles relax, your airway narrows or closes as you breath in and breathing may be inadequate for 10 to 20 seconds. This may lower the level of oxygen in your blood and cause a buildup of carbon dioxide.
Your brain senses this impaired breathing and briefly rouses you from sleep so that you can reopen your airway. This awakening is usually so brief that you don't remember it.
You can awaken with a transient shortness of breath that corrects itself quickly, within one or two deep breaths. You may make a snorting, choking or gasping sound.
This pattern can repeat itself five to 30 times or more each hour, all night long. These disruptions impair your ability to reach the desired deep, restful phases of sleep, and you'll probably feel sleepy during your waking hours.
People with obstructive sleep apnea may not be aware that their sleep was interrupted. In fact, many people with this type of sleep apnea think they slept well all night.
Risk factors
Anyone can develop obstructive sleep apnea. However, certain factors put you at increased risk, including:
- Excess weight. Around half the people with obstructive sleep apnea are overweight. Fat deposits around the upper airway may obstruct breathing.
However, not everyone with obstructive sleep apnea is overweight and vice versa. Thin people can also develop this disorder . - Narrowed airway. You may inherit naturally narrow airways. Or, your tonsils or adenoids may become enlarged, which can block your airway.
- High blood pressure (hypertension). Obstructive sleep apnea is relatively common in people with hypertension.
- Chronic nasal congestion. Obstructive sleep apnea occurs twice as often in those who have consistent nasal congestion at night, regardless of the cause. This may be due to narrowed airways.
- Smoking. People who smoke are more likely to have obstructive sleep apnea.
- Diabetes. Obstructive sleep apnea may be more common in people with diabetes.
- Sex. In general, men are twice as likely as women to have obstructive sleep apnea.
- Family history of sleep apnea. If you have family members with obstructive sleep apnea, you may be at increased risk.
- Asthma. Recent research has found an association between asthma and the risk of obstructive sleep apnea. Complications
Obstructive sleep apnea is considered a serious medical condition. Complications may include:
- Daytime fatigue and sleepiness. The repeated awakenings associated with obstructive sleep apnea make normal, restorative sleep impossible. People with obstructive sleep apnea often experience severe daytime drowsiness, fatigue and irritability. They may have difficulty concentrating and find themselves falling asleep at work, while watching TV or even when driving.
Children and young people with obstructive sleep apnea may do poorly in school and commonly have attention or behavior problems. - Cardiovascular problems. Sudden drops in blood oxygen levels that occur during obstructive sleep apnea increase blood pressure and strain the cardiovascular system. Many people with obstructive sleep apnea develop high blood pressure (hypertension), which can increase the risk of heart disease.
The more severe the obstructive sleep apnea, the greater the risk of Strokecoronary artery disease, heart attack and heart failure. Obstructive sleep apnea increases the risk of abnormal heart rhythms (arrhythmias). These abnormal rhythms can lower blood oxygen levels. If there's underlying heart disease, these repeated multiple episodes of low blood oxygen could lead to sudden death from a cardiac event. - Complications with medications and surgery. Obstructive sleep apnea also is a concern with certain medications and general anesthesia. These medications, such as sedatives, narcotic analgesics and general anesthetics, relax your upper airway and may worsen your obstructive sleep apnea.
If you have obstructive sleep apnea, you may experience worse breathing problems after major surgery, especially after being sedated and lying on your back. People with obstructive sleep apnea may be more prone to complications after surgery.
Before you have surgery, tell your doctor if you have obstructive sleep apnea or symptoms related to obstructive sleep apnea. If you have obstructive sleep apnea symptoms, your doctor may test you for obstructive sleep apnea prior to surgery. - Eye problems. Some research has found a connection between obstructive sleep apnea and certain eye conditions, such as glaucoma.
- Sleep-deprived partners. Loud snoring can keep those around you from getting good rest and eventually disrupt your relationships. Some partners may even choose to sleep in another room. Many bed partners of people who snore are sleep deprived as well.
People with obstructive sleep apnea may also complain of memory problems, morning headaches, mood swings or feelings of depression, and a need to urinate frequently at night (nocturia).
Signs and symptoms of obstructive sleep apnea include:
- Excessive daytime sleepiness
- Snoring loud enough to disturb your sleep or that of others
- Observed episodes of breathing cessation during sleep
- Abrupt awakenings accompanied by gasping or choking
- Awakening with a dry mouth or sore throat
- Morning headache
- Difficulty concentrating during the day
- Waking up gasping or choking
- Intermittent pauses in your breathing during sleep
- Excessive daytime drowsiness, which may cause you to fall asleep while you're working, watching television or even driving a vehicle
- Experiencing mood changes, such as depression or irritability
- High blood pressure
- Nighttime sweating
- Decreased libido
Many people may not think of snoring as a sign of something serious, and not everyone who snores has obstructive sleep apnea.
Be sure to talk to your doctor if you experience loud snoring, especially snoring that's punctuated by periods of silence. With obstructive sleep apnea, snoring usually is loudest when you sleep on your back, and it quiets when you turn on your side.
Ask your doctor about any sleep problem that leaves you chronically fatigued, sleepy and irritable. Excessive daytime drowsiness may be due to other disorders, such as narcolepsy.
Parkinson's Disease
Parkinson's disease (PD) is a neurodegenerative disorder that affects predominately dopamine-producing (“dopaminergic”) neurons in a specific area of the brain called substantianigra.
Symptoms generally develop slowly over years. The progression of symptoms is often a bit different from one person to another due to the diversity of the disease. People with PD may experience:
The cause remains largely unknown. Other than medicinal treatment there are also other modes of therapy including surgery. While Parkinson’s itself is not fatal, disease complications can be serious. It is important to remember that two of the four main symptoms must be present over a period of time for a neurologist to consider a PD diagnosis:
- • Shaking or tremor
- • Slowness of movement, called bradykinesia
- • Stiffness or rigidity of the arms, legs or trunk
- • Trouble with balance and possible falls, also called postural instability
Below are 10 signs that you might have the disease. No single one of these signs means that you should worry, but if you have more than one sign you should consider making an appointment with a neurologist.
Tremor
Have you noticed a slight shaking or tremor in your finger, thumb, hand or chin? A tremor while at rest is a common early sign of Parkinson's disease.
Small Handwriting
Has your handwriting gotten much smaller than it was in the past? You may notice the way you write words on a page has changed, such as letter sizes are smaller and the words are crowded together. A change in handwriting may be a sign of Parkinson's disease called micrographia.
Loss of Smell
Have you noticed you no longer smell certain foods very well? If you seem to have more trouble smelling foods like bananas, dill pickles or licorice, you should ask your doctor about Parkinson's.
Trouble Sleeping
Do you thrash around in bed or act out dreams when you are deeply asleep? Sometimes, your spouse will notice or will want to move to another bed. Sudden movements during sleep may be a sign of Parkinson's disease.
Trouble Moving or Walking
Do you feel stiff in your body, arms or legs? Have others noticed that your arms don’t swing like they used to when you walk? Sometimes stiffness goes away as you move. If it does not, it can be a sign of Parkinson's disease. An early sign might be stiffness or pain in your shoulder or hips. People sometimes say their feet seem “stuck to the floor.”
Constipation
Do you have trouble moving your bowels without straining every day? Straining to move your bowels can be an early sign of Parkinson's disease and you should talk to your doctor.
A Soft or Low Voice
Have other people told you that your voice is very soft or that you sound hoarse? If there has been a change in your voice you should see your doctor about whether it could be Parkinson's disease. Sometimes you might think other people are losing their hearing, when really you are speaking more softly.
Masked Face
Have you been told that you have a serious, depressed or mad look on your face, even when you are not in a bad mood? This is often called facial masking. If so, you should ask your doctor about Parkinson's disease.
Dizziness or Fainting
Do you notice that you often feel dizzy when you stand up out of a chair? Feeling dizzy or fainting can be a sign of low blood pressure and can be linked to Parkinson's disease (PD).
Stooping or Hunching Over
Are you not standing up as straight as you used to? If you or your family or friends notice that you seem to be stoopingor leaning when you stand, it could be a sign of Parkinson's disease (PD).
Treatment for each person with Parkinson's is based on his or her symptoms.
Treatments include medication and surgical therapy. Other treatments include lifestyle modifications, like getting more rest and exercise.
There are many medications available to treat the Parkinson’s symptoms, although none of them reverse the effects of the disease. It is common for people with PD to take a variety of these medications — all at different doses and at different times of day — to manage symptoms.
While keeping track of medications can be a challenging task, understanding your medications and sticking to a schedule will provide the greatest benefit from the drugs and avoid unpleasant “off” periods due to missed doses.
Peripheral Neuropathy
It’s hard to identify peripheral neuropathy as a single disease. However, most experts use it as a general term to refer to a series of disorders that can result because of damage to the peripheral nervous system. This system sends messages from the spinal cord and brain to the remainder of the body, including the feet and legs, hands, and arms, joints, organs, and even the skin. Peripheral nerves are also responsible for relaying information back to the brain and spinal cord from those various places. The symptoms of peripheral neuropathy take place when the nerves are destroyed or damaged. Peripheral neuropathy has something of a variable course, and it can come and go, progressing slowly over a number of years. However, if it is diagnosed early, peripheral neuropathy can be controlled, and even cured in some cases
There are a number of different things responsible for peripheral neuropathy , including hereditary disorders, diabetes, inflammation, autoimmune disease, infections, compression, protein abnormalities, and physical trauma. Some people experience neuropathy as a result of poor nutrition,vitamin deficiencies, toxins & chemicals, alcoholism, or exposure to certain medication, particularly those used in chemotherapy treatments for cancer. However, in some cases, even with an in-depth evaluation, the causes of a person’s neuropathy may remain unknown.
Literally all of the areas within the body, apart from the central nervous system and brain, can be affected by peripheral neuropathy. Think for a moment about which parts of the body don’t have peripheral nerves, and you’ll come up with nothing more than the central nervous system and the brain. In other words, your neuropathy problem can impact everything from the vascular system, to the digestive tract, and more. However, most commonly it appears within the feet and legs.
While each person is likely to experience peripheral neuropathy in a different way, there are some common signs and symptoms that can be associated with this condition. For instance, at first you’re likely to experience abnormal sensations, pain, tingling, or numbness in certain parts of your body. Some people feel as though they have socks on even though their feet are bare. Over time, the feeling can spread from your feet to your hands and legs.
In some cases, people with peripheral neuropathy find it harder to walk normally because their legs feel heavier, and they need to drag themselves up and down the stairs. Sometimes, they may notice that they begin to lose their balance, or struggle to figure out where their feet are in conjunction with their legs. As for hands, some people find that even when they think they have a good grip on something, they end up dropping them straight away.
The signs and symptoms of peripheral neuropathy can often vary in how they begin to appear. Some neuropathies come on all of a sudden, whereas others appear gradually over a number of years. There are three types of peripheral nerves that can be affected, and the symptoms will depend on these nerves and their location. For instance, your sensory nerves will affect sensation, whereas your autonomic nerves affect internal organ function, and your motor nerves affect muscles.
Neurologists call this issue the length dependent affect. Basically, if you think of your body as a string of wires that carry electricity, it will take more energy for the current that starts at the top of your head, in your brain, to reach the feet, because of the length of wire that needs to be travelled. In other words, this means that there is more push required in getting signals from the brain to the feet. If there is damage along the lines of the nervous system, chances are that the feet will feel the impact before other areas in the body.
Of course, in some less than typical forms of neuropathy, other parts of the body may be impacted first because of the location and causes of the damage to the peripheral nerves.
Yes ,Other than clinical examination we can also diagnose neuropathy by doing Nerve Conduction Velocity test also known as NCV test .
It is important to know that some forms of peripheral neuropathy can be cured, but some can also not be cured. However, it’s also important to know that many patients can help their symptoms by taking a range of treatments. Therapies for peripheral neuropathy are often directed towards treating the underlying cause of the problem with the right medications. For instance, someone who experiences peripheral neuropathy as a result of diabetes may need to work on managing their diabetes and blood sugar level before trying any other form of treatment.
However, with that in mind, recent research has begun to show some positive results when it comes to tracking down treatments for neuropathies.
The reason for this is that vitamins and nutrients, such as B12 and alpha linolenic acid, are known to be effective when it comes to repairing the pathways in nerves and helping to promote the reduction of symptoms. When used in the right combination, an array of vitamins can help to reduce the most common symptoms associated with neuropathy, from the burning and tearing pains that are sent by misfiring nerves, to the tingling and numbness that can occur as a result of damaged nerves being unable to pick up sensation as they should.
Moreover there are other medicines prescribed by neurologist to modify & repair the nerves responsible for painful symptoms .



